By Dr. David Stewart
By Dr. David Stewart
In this blog series, we present excerpts from Dr. David Stewart’s book A Short Primer on Why Cancer Still Sucks. If you would like to read Dr. Stewart’s 13 other reasons, plus what the future of cancer research might look like, copies are available through Amazon Books or at whycancerstillsucks.com.
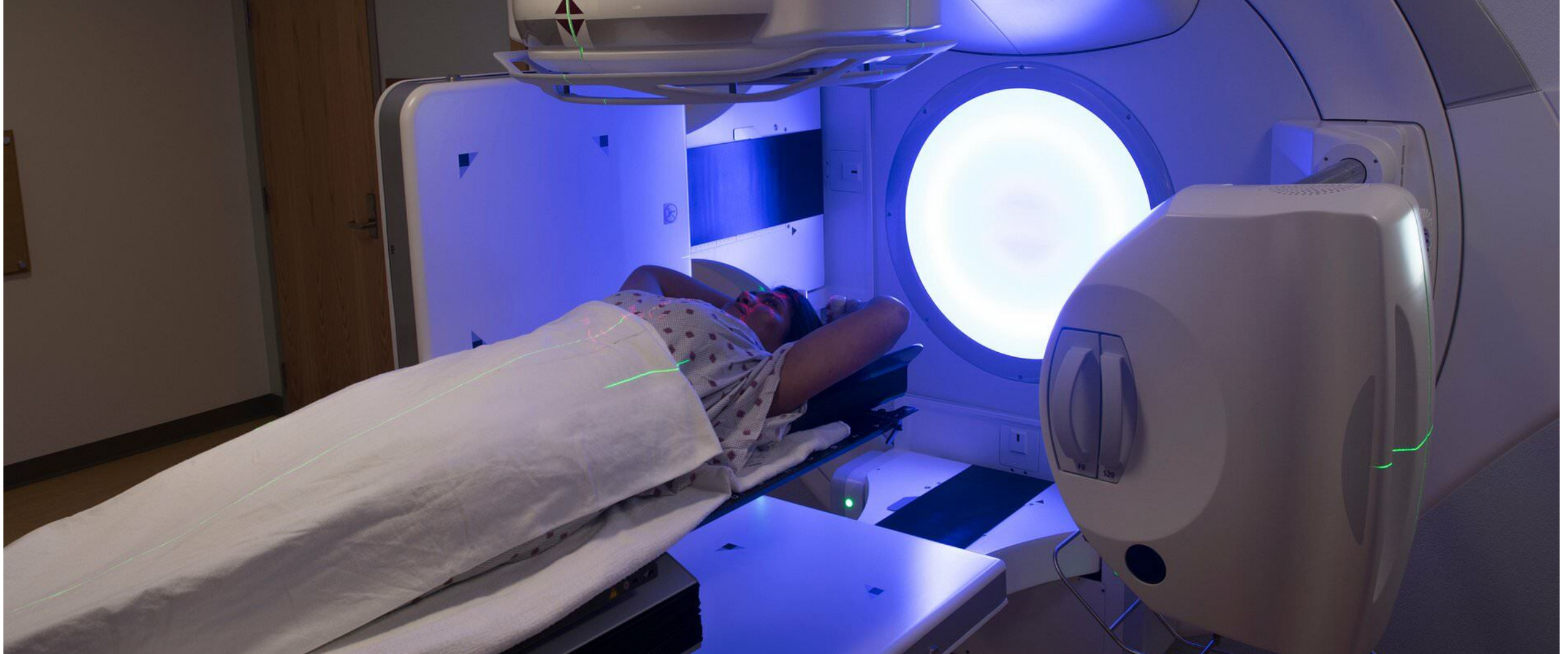
The fifth reason that cancer still sucks is that although radiation therapy can be an effective cancer treatment, it may fail to kill some of the tumor cells in its path, or it may miss some tumor cells completely. In addition, while “palliative” radiotherapy can dramatically improve symptoms in some individuals with incurable cancers, it may have minimal impact or provide only very brief relief to others.
Benefits of radiotherapy
Radiotherapy can cure some localized cancers that are not amenable to surgery. With surgery, the entire tumor mass may be removed, while with radiotherapy, a small number of tumor cells within the tumor mass may survive the treatment. However, radiotherapy is an option when surgery is not feasible, and it unequivocally can cure many patients with localized cancers. If administered following surgery, radiotherapy may also reduce the risk of a cancer recurring In selected patients with incurable cancers, it can also be highly effective in improving cancer symptoms like pain, shortness of breath, and bleeding.
How radiotherapy works
Radiotherapy acts like a bolt of lightning that breaks DNA in tumor cells. This DNA damage can either kill the cell or can cause changes that prevent the cell from dividing again. Some of the DNA damage caused by radiotherapy can be repaired. Normal cells are somewhat more effective at repairing the damage than tumor cells, particularly when relatively low doses of radiation are given.
This is why “curative intent” radiation is often given once or twice per day, Monday to Friday for several weeks in a row. The day-to-day cumulative DNA damage in tumor cells may be greater than in normal cells since the tumor cells do not do as good a job in repairing DNA damage as the normal cells. The result can be eradication of the tumor without excessive toxicity to normal tissues. Some, but not all the DNA damage in normal cells will be repaired. If a cancer grows back in an area that was previously treated with high dose radiotherapy, a patient might tolerate a low dose of additional radiotherapy to try to temporarily reduce symptoms. However, they could not be treated again with a high dose of radiotherapy since it could cause permanent, severe, disabling, or life-threatening damage to skin, major blood vessels, or other organs. Because of this permanent tissue damage, radiation oncologists carefully keep track of the areas they have treated and of the radiation doses these areas have received.
Surgery is also often not an option for a tumor that has recurred in a previously radiated area. Tissues that have received high dose radiotherapy do not heal well after surgery. Radiation-induced scarring also makes the tissue very hard and difficult to remove. It also is difficult to see and maneuver around major blood vessels during surgery in regions of the body that have been radiated. Doing surgery in these areas carries an increased risk of major, life-threatening bleeding. If a team starts out with a plan to give high-dose radiotherapy followed by surgery, they will try to ensure whether the radiotherapy will help. Their decision will depend on a variety of factors, such as the mechanism by which the cancer is causing the symptom, the type of cancer, etc. In addition to decide if radiation will help, they will also ensure that the surgery is done within just a few weeks after completion of the radiotherapy before substantial scar tissue has formed.
Why radiotherapy may fail
Radiotherapy may fail because some stubborn tumor cells unfortunately can repair the DNA damage caused by radiotherapy. In addition, “hypoxic” tissues (tissues that are oxygen deficient) have increased resistance to radiotherapy. Large tumors are more likely than small tumors to have hypoxic areas. Thus, they are less likely to be cured by radiotherapy. In addition, a large tumor has a higher number of tumor cells than a small tumor. Consequently, it is more likely to have cells with resistance causing mutations or cells that escape into the blood stream to cause incurable distant metastases. Only a very small fraction of tumor cells may have developed resistance inducing mutations. But if just one out of a billion cancer cells survives the radiation, the tumor eventually regrows. These regrowing cells may be resistant to further radiotherapy since they inherited these resistance inducing mutations.
Rapidly growing tumor cells are more sensitive to radiotherapy than slowly growing cells. But if the cells grow very rapidly, all the cells that were killed by a radiotherapy treatment may already have been replaced by new cells by the time the next treatment is given the following day. Antioxidants like vitamins C and E can also increase the resistance of tumor cells to radiotherapy.
Lastly, tumor location can play a role in the success of radiotherapy. Take as an example a patient with a cancer at the bottom of the lung that has spread to lymph nodes high up in the chest. To treat all the metastasized areas, radiotherapy would need to hit a large area which could mean hitting too large an amount of normal lung tissue. Also, certain areas, such as the liver, spinal cord, intestine, and heart, are very sensitive, making it hard to safely use radiotherapy in those areas.
Drugs that increase sensitivity of cancers to radiotherapy
Combining some chemotherapy agents with radiotherapy can make for a better treatment plan. For many cancers, it is now the standard of care to combine selected chemotherapy agents with “curative intent” high-dose radiotherapy. Not only may the chemotherapy make radiotherapy more effective in the areas that the radiation hits, but it also may kill very small tumor deposits (too small to show up on scans) outside of the area treated by the radiotherapy.