By continuing to use our site, you consent to the processing of cookies, user data (location information, type and version of the OS, the type and version of the browser, the type of device and the resolution of its screen, the source of where the user came from, from which site or for what advertisement, language OS and Browser, which pages are opened and to which buttons the user presses, ip-address) for the purpose of site functioning, retargeting and statistical surveys and reviews. If you do not want your data to be processed, please leave the site.
The Voice of People With Breast Cancer
Information
Breast Cancer Basics
Diagnosing Breast Cancer
Breast cancer can be found either through routine screening before any symptoms appear or after symptoms develop. To make a diagnosis, healthcare providers use a variety of methods including physical exams, imaging tests and biopsies.
Medical History and Physical Exams
When checking your breast health, your healthcare provider will ask about your medical history, including symptoms, personal and family history of breast or other cancers and any other known risk factors.
A clinical breast exam (CBE) may be performed to check for lumps or other changes. The exam includes:
- Checking the skin for changes in texture, size, or shape
- Feeling for lumps or irregularities in the breast and underarms
- Assessing lymph nodes under the arms and collarbone
Clinical breast exams are typically used if you have symptoms, a family history of breast cancer, or other risk factors. While a CBE can help detect some lumps or irregularities, it may not catch small cancers that imaging can detect. It’s also important to know that a normal CBE doesn’t rule out breast cancer. If you have ongoing symptoms, additional imaging may still be recommended.
Imaging Tests
Imaging helps healthcare providers examine breast tissue for signs of cancer.
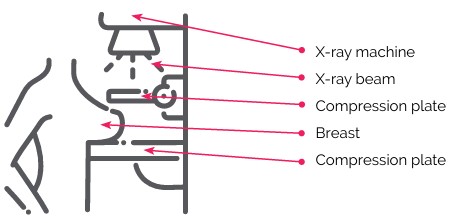
Mammography
A mammogram is a specialized X-ray that detects changes in breast tissue, such as small lumps or calcifications that cannot be felt by hand. Mammograms are considered safe, as they use low-dose radiation.
Diagnostic Mammography is used if a screening mammogram detects irregularities or if symptoms are present. It provides more detailed images and can help guide a biopsy.
A new screening tool, digital tomosynthesis (3D mammography), is available in some areas. This technology provides more detailed, three-dimensional images, improving cancer detection in dense breast tissue.
Ultrasound
A breast ultrasound uses sound waves to create images of the breast. It is often used alongside a mammogram to:
- Evaluate breast lumps or abnormalities
- Distinguish between solid tumours and fluid-filled cysts
- Guide a biopsy
Breast MRI (Magnetic Resonance Imaging)
A breast MRI uses magnetic fields and radio waves to create detailed, three-dimensional images of the breast. It does not use radiation and is used to:
- Evaluate abnormal areas when mammogram or ultrasound results are inconclusive
- Detect hereditary breast cancer in high-risk individuals (e.g., BRCA1 or BRCA2 mutations)
- Investigate nipple discharge or suspected distant metastases
- Screen people with dense breasts, as it may detect cancers missed by mammograms
PET (Positron Emission Tomography) Scan
A PET scan uses a small amount of radioactive material to take detailed pictures of how your organs and tissues are working. Cancer cells often absorb more of this material than normal cells, so areas with cancer show up more clearly on the scan.
PET scans are not commonly used to diagnose or stage early breast cancer (stage I or II). It may be recommended if:
- The cancer is more advanced (stage III or inflammatory)
- Your doctor suspects the cancer has spread to other parts of the body (known as metastatic breast cancer)
- Results from other imaging tests are unclear
Wait times for imaging vary. Ask your doctor about referral timelines or cancellation lists.
Biopsy
A biopsy removes a sample of breast tissue or cells for examination under a microscope. It is the only definitive way to confirm breast cancer. The type of biopsy performed depends on whether the abnormal area is palpable (can be felt) or non-palpable (detected only through imaging).
Types of breast biopsies include:
- Fine Needle Aspiration (FNA): Uses a thin needle to extract fluid or cells, often to determine if a lump is a cyst or solid mass. However, it cannot confirm if cancer is invasive.
- Core-Needle Biopsy: Uses a thin, hollow needle to remove small tissue samples, often guided by imaging such as ultrasound, mammography, or MRI.
- Stereotactic Core Biopsy: Uses 3D imaging to precisely locate and sample an abnormality that is visible on imaging but cannot be felt.
- Vacuum-Assisted Core Biopsy: A variation of core-needle biopsy that uses suction to remove a larger tissue sample.
- Wire Localization Biopsy: Involves placing a thin wire into an abnormal breast area using mammography to guide a surgical biopsy.
- Punch Biopsy: Uses a hollow instrument to remove a sample of skin and underlying tissue, often to diagnose inflammatory breast cancer.
- Surgical (Open) Biopsy: A surgeon removes part or all of a suspicious lump for further analysis. This includes:
- Excisional Biopsy: Removes the entire abnormal area along with a margin of healthy tissue.
- Incisional Biopsy: Removes only a portion of the abnormal area for examination.
Types of lymph node biopsies include:
- Sentinel Lymph Node Biopsy (SLNB): Identifies and removes the first lymph node(s) where cancer is likely to spread. Additional nodes are removed only if cancer is detected.
- Axillary Lymph Node Dissection (ALND): Removes multiple lymph nodes under the arm to assess cancer spread, typically when cancer has already been found in the lymph nodes.
Your healthcare provider will determine the most appropriate biopsy method based on the size, location, and characteristics of the abnormal area.
Biopsy Results & Follow-Up
Biopsy results are usually available within 7 days and provide important details such as:
- Cell type and grade – Helps determine how aggressive the cancer is.
- Hormone receptor status (ER, PR, HER2) – Guides treatment options.
Read more about what is included in a pathology report here.
If further staging is needed, your doctor may recommend additional imaging, such as a chest X-ray, CT scan, or bone scan, to assess whether cancer has spread.
Medical Review by Roochi Arora, MD, FRCPC, August 2025
- References
-
Canadian Breast Cancer Network. (2022). Breast cancer and you: A guide for people living with breast cancer [PDF]. https://cbcn.ca/web/default/files/public/
Reports/Breast%20Cancer%20and%20You_
ENG_edit_web.pdfCanadian Cancer Society. (2024). Screening for breast cancer. https://cancer.ca/en/cancer-information/cancer-types/breast/screening
Canadian Cancer Society. (2024). Mammography. https://cancer.ca/en/treatments/tests-and-procedures/mammography
Canadian Cancer Society. (n.d.). Diagnosis of breast cancer. https://cancer.ca/en/cancer-information/cancer-types/breast/diagnosis
Canadian Task Force on Preventive Health Care. (2024). Breast cancer: Draft recommendations for screening. https://canadiantaskforce.ca/breast-cancer-update-draft-recommendations/
Cao, J. Q., Surgeoner, B., Manna, M., et al. (2024). Guidance for Canadian breast cancer practice: National consensus recommendations for clinical staging of patients newly diagnosed with breast cancer. Current Oncology, 31(11), 7226-7243. https://doi.org/10.3390/curroncol31110533
Cleveland Clinic. (2023). PET scan: Purpose, procedure, risks & results. Cleveland Clinic. https://my.clevelandclinic.org/health/
diagnostics/10123-pet-scanKleinknecht, J. H., Ciurea, A. I., & Ciortea, C. A. (2020). Pros and cons for breast cancer screening with tomosynthesis - A review of the literature. Medicine and Pharmacy Reports, 93(4), 335–341. https://doi.org/10.15386/mpr-1698
SHARE