By continuing to use our site, you consent to the processing of cookies, user data (location information, type and version of the OS, the type and version of the browser, the type of device and the resolution of its screen, the source of where the user came from, from which site or for what advertisement, language OS and Browser, which pages are opened and to which buttons the user presses, ip-address) for the purpose of site functioning, retargeting and statistical surveys and reviews. If you do not want your data to be processed, please leave the site.
The Voice of People With Breast Cancer
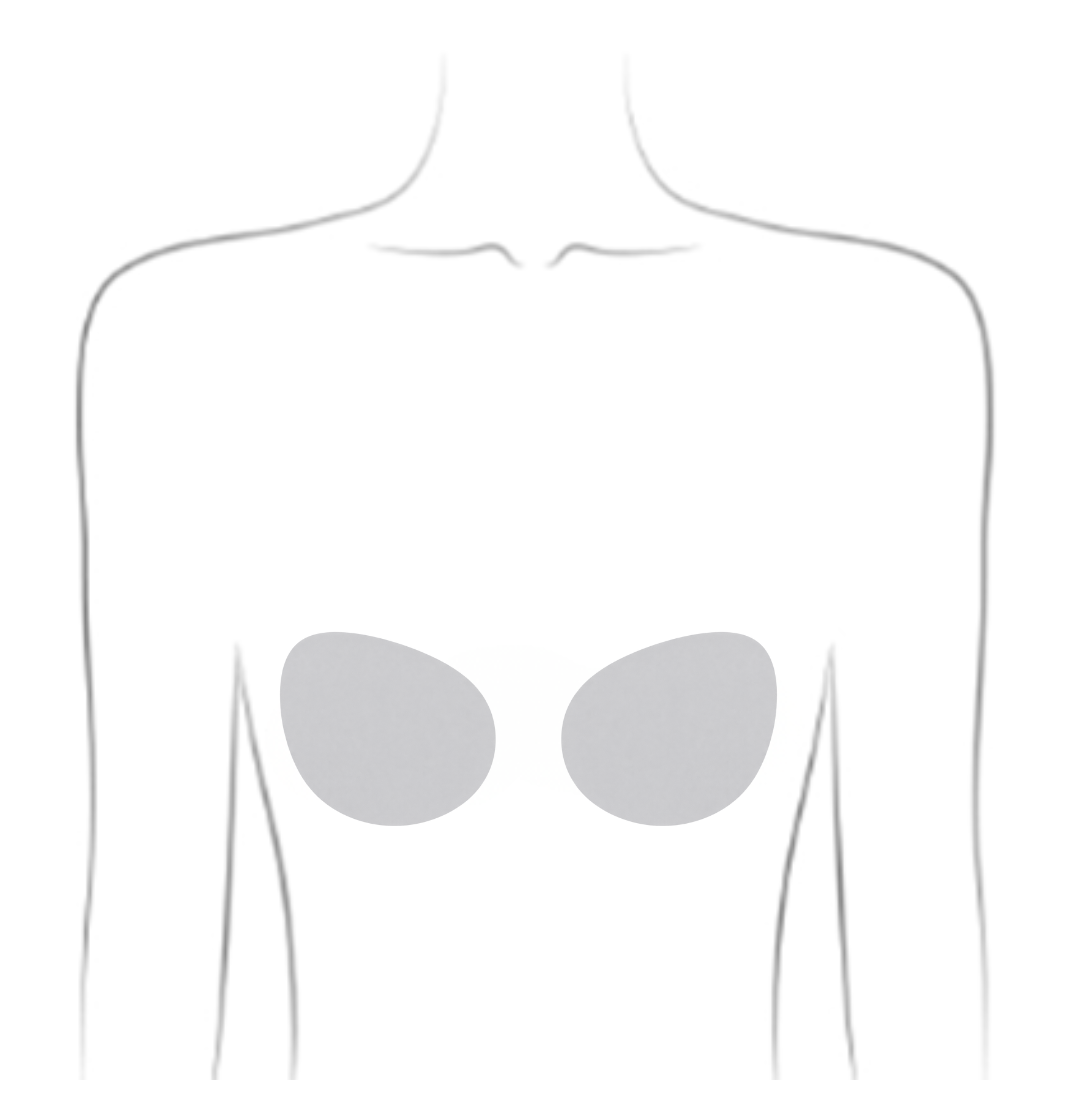
helping you understand your surgical options
SurgeryGuide
Jump to:
Mastectomy
A mastectomy is the surgical removal of the entire breast. It may be recommended as part of breast cancer treatment or used to lower the risk of cancer for people with a high genetic risk.
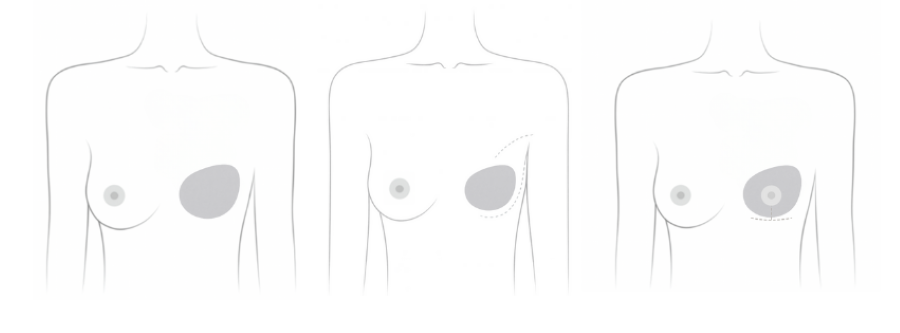
Types of Mastectomies
Different types of mastectomies are available depending on your diagnosis, treatment plan, and personal preferences.
-
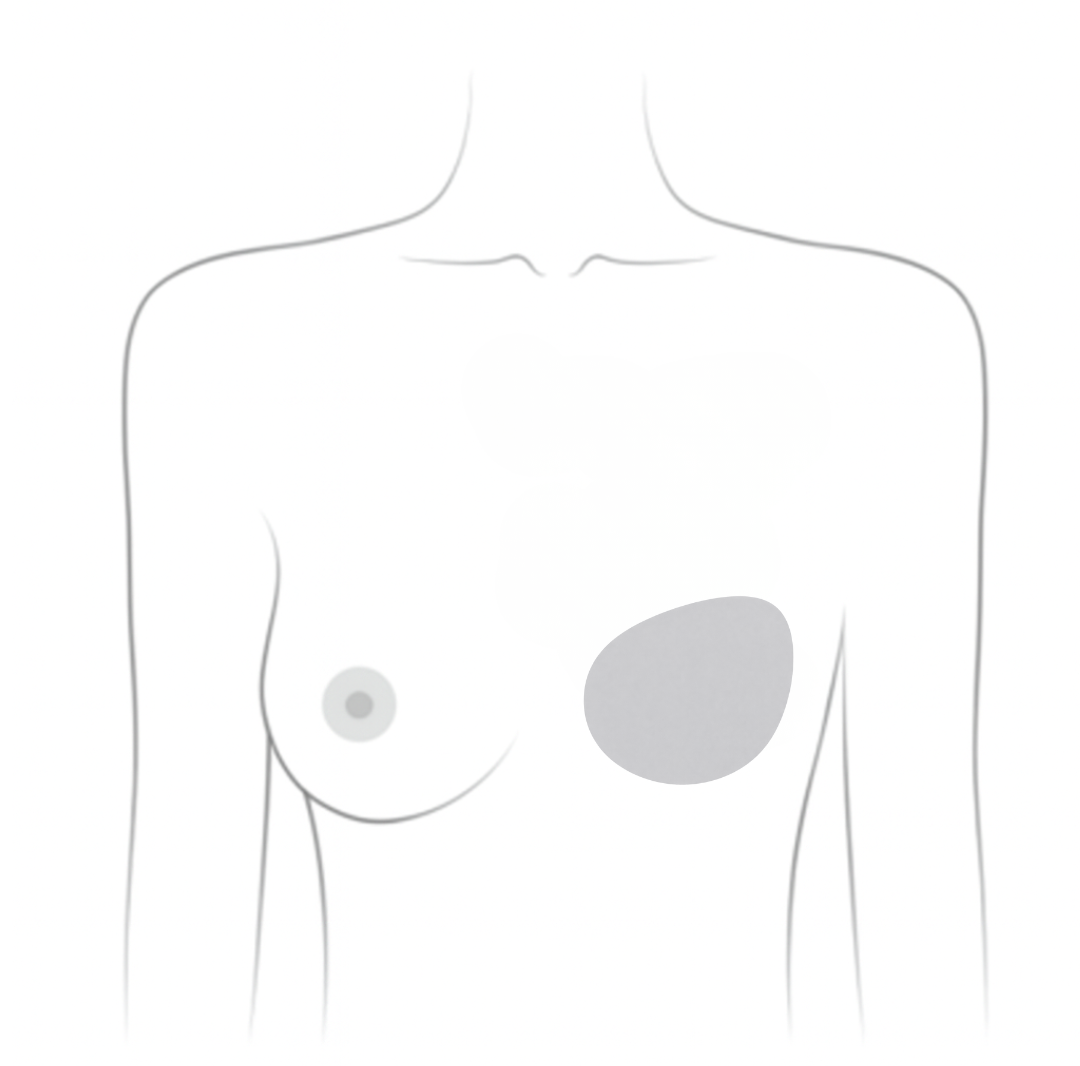
Total (Simple) Mastectomy
Removes the entire breast, including the nipple and areola. Lymph nodes may be removed at the same time
May be recommended if you:
- Have ductal carcinoma in situ (DCIS) or early-stage invasive breast cancer
- Are not planning reconstruction right away
- Prefer a flat closure or prosthetic instead of reconstruction
-
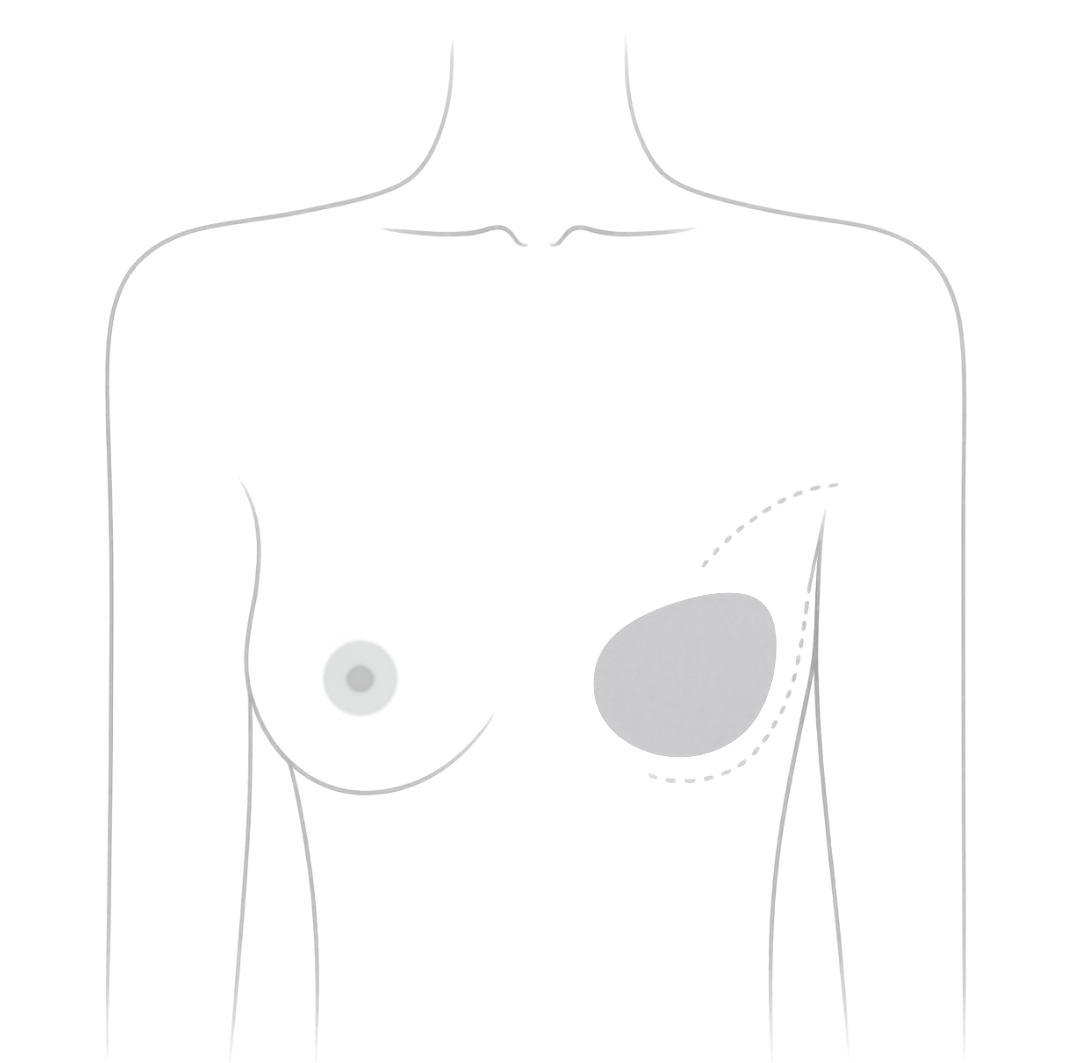
Skin-Sparing Mastectomy (SSM)
Removes breast tissue, nipple, and often the areola, but keeps most of the natural breast skin
May be recommended if you:
- Commonly done when immediate reconstruction is planned
- keeping the skin can help create a more natural-looking reconstruction
-
May not be recommended if:
- Cancer involves or is close to the skin
- You have been diagnosed with inflammatory breast cancer
If needed, lymph node removal is typically done during the same surgery.
-
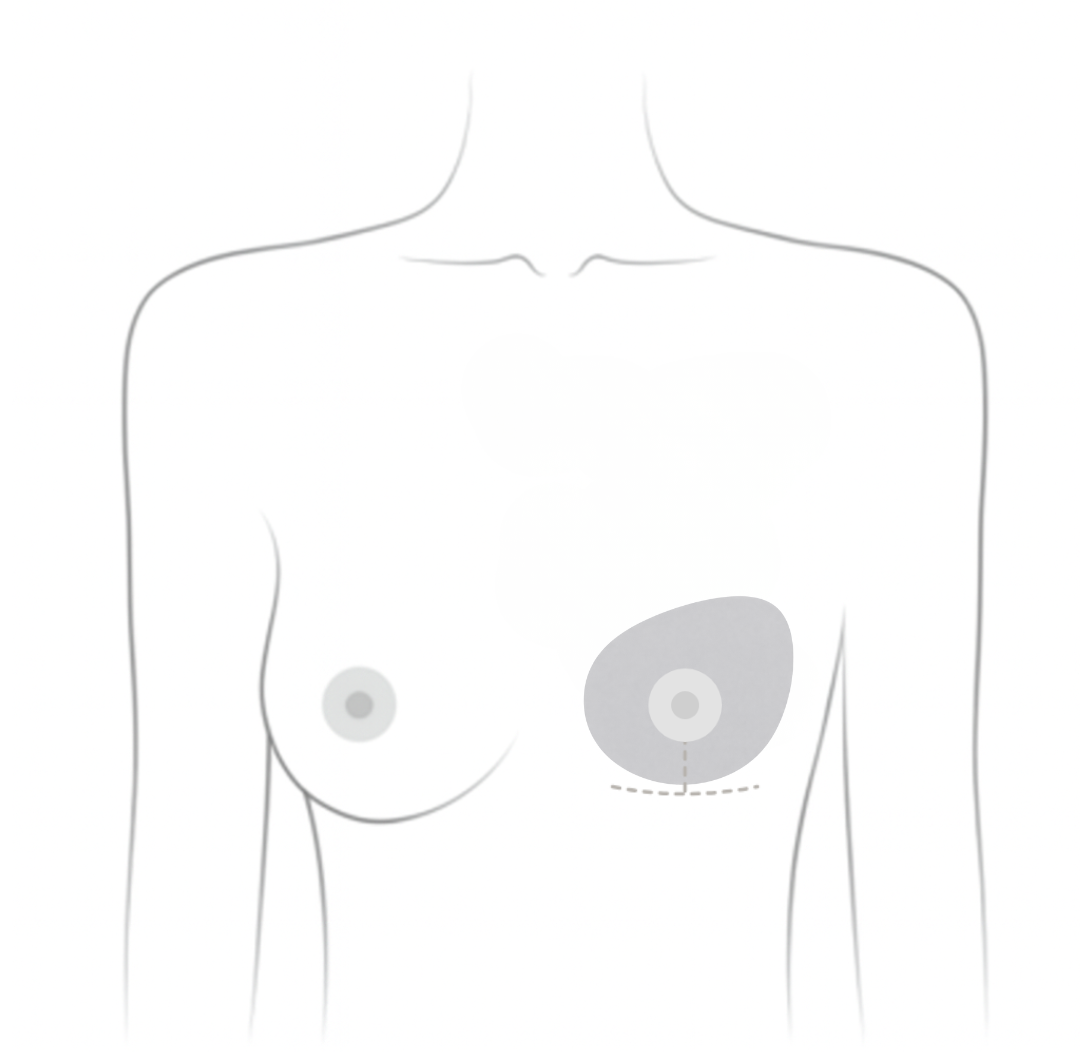
Nipple-Sparing Mastectomy (NSM)
Removes breast tissue while preserving the nipple, areola, and most of the breast skin. Usually combined with immediate reconstruction
May be recommended if you:
- Have early-stage breast cancer best treated with a mastectomy
- Have no cancer near or involving the nipple
Keeping the nipple may help emotional well-being and give more natural looking results. However, NSM requires careful planning and surgical skill to ensure proper blood supply to the nipple.
NSM is not available in all regions and may depend on your surgeon’s training and a plastic surgeon’s availability. When appropriately selected, the risk of cancer recurrence in the nipple area is low.
Click here to see before and after photos of real people.
Related reading from Our Voices Blog:
Coverage for Prophylactic Mastectomy
In Canada, prophylactic mastectomy is publicly funded for individuals with a BRCA mutation or those considered high risk. However, eligibility criteria vary by province. Speak with your healthcare provider to determine your coverage options.
Coverage also varies for patients with cancer in one breast who wish to remove the other. In most cases, the decision is made between the patient and physician based on individual circumstances.
Medical Reviews by Siba Haykal, MD, PhD, FRCSC, FACS, October 2025 and Mark Basik, MD, FRCSC, December 2025
- References
-
Canadian Breast Cancer Network. (2022). Breast cancer and you: a guide for people living with breast cancer [PDF]. https://cbcn.ca/web/default/files/public/Reports/Breast%20Cancer%20and%20You_ENG_edit_web.pdf
Canadian Cancer Society. (2023). Breast prostheses. https://cancer.ca/en/cancer-information/cancer-types/breast/reconstruction-and-prostheses/breast-prostheses
Canadian Cancer Society. (2023). Breast reconstruction. https://cancer.ca/en/cancer-information/cancer-types/breast/reconstruction-and-prostheses/breast-reconstruction-surgery
Canadian Cancer Society. (2023). Choosing to remain flat. https://cancer.ca/en/cancer-information/cancer-types/breast/reconstruction-and-prostheses/choosing-to-remain-flat
Center for Restorative Breast Surgery. (n.d.). Nipple sparing mastectomy. https://www.breastcenter.com/breast-reconstruction-procedures/nipple-sparing-mastectomy/
Conner, K. (2025). Going flat after mastectomy. Breastcancer.org. https://www.breastcancer.org/treatment/surgery/going-flat-no-reconstruction
Galimberti, V., Vicini, E., Corso, G., Morigi, C., Fontana, S., Sacchini, V., & Veronesi, P. (2017). Nipple-sparing and skin-sparing mastectomy: Review of aims, oncological safety and contraindications. Breast (Edinburgh, Scotland), 34 Suppl 1(Suppl 1), S82–S84. https://doi.org/10.1016/j.breast.2017.06.034
Knitted Knockers Canada. (2025). Soft, comfortable, knit prosthetics for breast cancer survivors. https://knittedknockerscanada.com/
National Cancer Institute. (2025). Breast reconstruction after mastectomy. National Institutes of Health. https://www.cancer.gov/types/breast/reconstruction-fact-sheet
Nelson, R. (n.d.). Nipple sparing mastectomy: Tips & tricks. BC Cancer. http://www.bccancer.bc.ca/surgical-oncology-network-site/Documents/Rebecca%20Nelson%20-%20Nipple%20Sparing%20Mastectomy%20Tips%20and%20Tricks.pdf
Susan G. Komen. (2025). Breast reconstruction. https://www.komen.org/breast-cancer/treatment/type/surgery/breast-reconstruction/
Uscher, J. (2024). Types of mastectomy. Breastcancer.org. https://www.breastcancer.org/treatment/surgery/mastectomy/types
Wu, Z. Y., Kim, H. J., Lee, J. W., Chung, I. Y., Kim, J. S., Lee, S. B., Son, B. H., Eom, J. S., Kim, S. B., Gong, G. Y., Kim, H. H., Ahn, S. H., & Ko, B. (2019). Breast cancer recurrence in the nipple-areola complex after nipple-sparing mastectomy with immediate breast reconstruction for invasive breast cancer. JAMA Surgery, 154(11), 1030–1037. https://doi.org/10.1001/jamasurg.2019.2959