By continuing to use our site, you consent to the processing of cookies, user data (location information, type and version of the OS, the type and version of the browser, the type of device and the resolution of its screen, the source of where the user came from, from which site or for what advertisement, language OS and Browser, which pages are opened and to which buttons the user presses, ip-address) for the purpose of site functioning, retargeting and statistical surveys and reviews. If you do not want your data to be processed, please leave the site.
The Voice of People With Breast Cancer
helping you understand your surgical options
SurgeryGuide
Jump to:
Making Decisions
Every breast cancer diagnosis is different, and so is every treatment plan. While you may meet others going through similar experiences, your care decisions are unique to you.
For additional guidance on choosing the right surgery, read CBCN Advocacy Guide: Deciding Which Breast Cancer Surgery is Right for You?
Things to Consider When Choosing Surgery
Age and Health
Your age and overall health can play a role in what surgery and post-surgery options are available to you. For example, certain surgeries like breast reconstruction may carry a higher risk of complications depending on these factors. Discuss your options with your doctor to determine what is best for you.
Where You Live
Where you live may impact your breast cancer surgery options.
-
Lumpectomy and radiation: Lumpectomy is often followed by radiation therapy, which requires visits to a cancer centre for several days, sometimes weeks. If you live far from a centre and would need to stay away from home, this may be a factor in choosing between lumpectomy and mastectomy.
- Reconstruction: Access to reconstruction depends on what is offered in your area. Some types of reconstruction may not be available nearby and you may need to travel to another city or province. Discuss your options with your healthcare team to determine what is feasible for you.
If you are thinking about lumpectomy or single mastectomy, discuss future screening options with your surgeon. Guidelines and imaging availability vary by province.
Comparing Lumpectomy & Mastectomy
If you have a smaller tumour, your surgeon may offer you a choice between lumpectomy (breast-conserving surgery) and mastectomy. For larger tumours, more advanced cancer, or cancer in multiple areas of the breast, mastectomy may be recommended.
Lumpectomy followed by radiation offers the same long-term survival as mastectomy. However, mastectomy may, in some cases, eliminate the need for radiation. Your decision should be based on your comfort, the specifics of your cancer, and guidance from your care team.
It’s important to know you do not have to rush this decision. While it is natural to want to act quickly, in most cases, it is safe to take a few weeks to explore your options and talk them through with your healthcare team.
The sections below outline the key differences between surgical options to help you make an informed choice.
Lumpectomy (Breast Conserving Surgery)
Removes part of the breast tissue instead of the whole breast
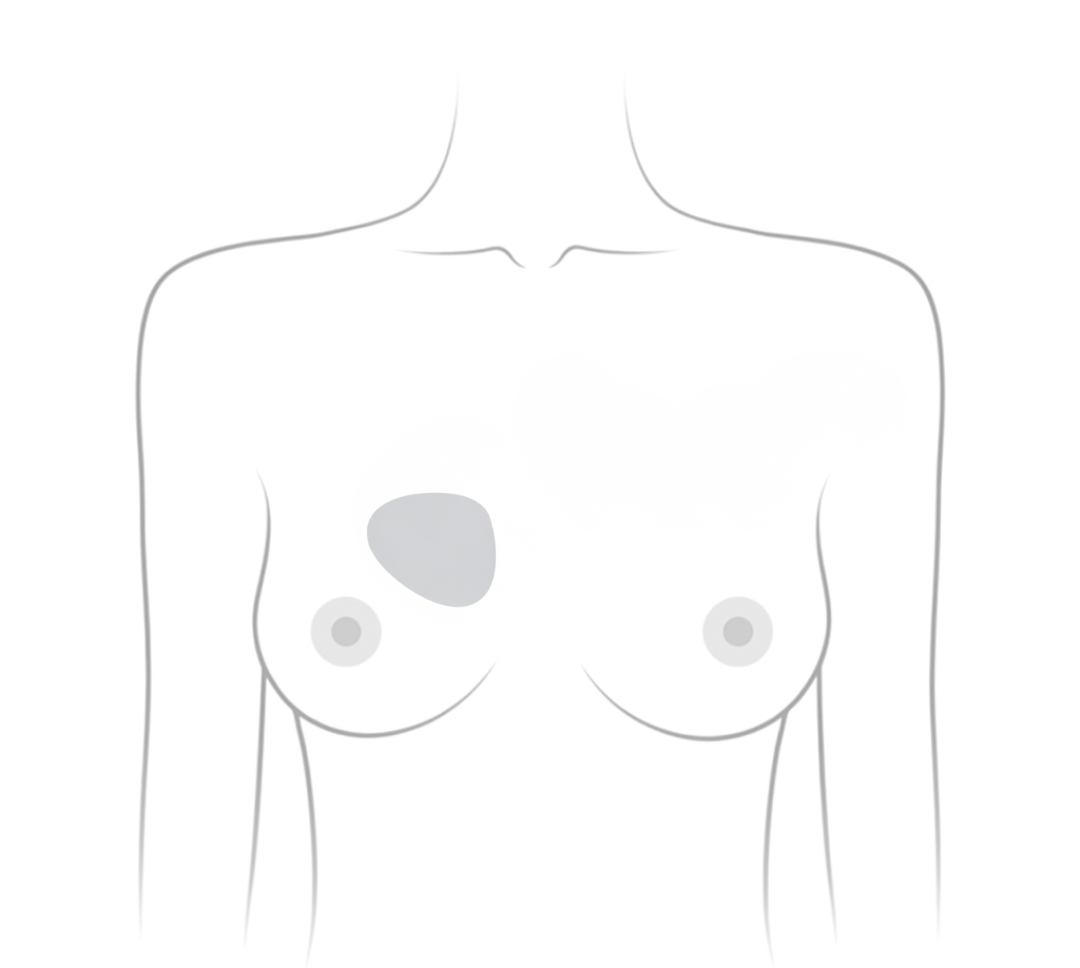
- Also called breast-conserving surgery or partial mastectomy
- May change the shape of the breast
- Reconstruction may be an option if a large amount of tissue is removed
- Newer “oncoplastic” approaches can partially or fully restore the shape of the breast and sometimes can compensate for the decrease in size of the breast with the cancer, by operating on the other breast to make them more equal or symmetrical.
- Shorter recovery time than mastectomy
- Radiation therapy is usually required after surgery
- A second surgery (margin revision) may be needed if margins are not clear (cancer cells are found at the edge of the removed tissue)
- In rare cases, a mastectomy may still be needed if margins continue not to be clear

“I had a lumpectomy first and when the pathologist determined that he was not happy with the margins, the surgeon had to go in and remove more breast tissue. He called it a partial mastectomy. Frankly, given that I had very small breasts to begin with, there wasn’t much left after the second surgery, although it was not a mastectomy.
~Karen~
Mastectomy
Removes the entire breast
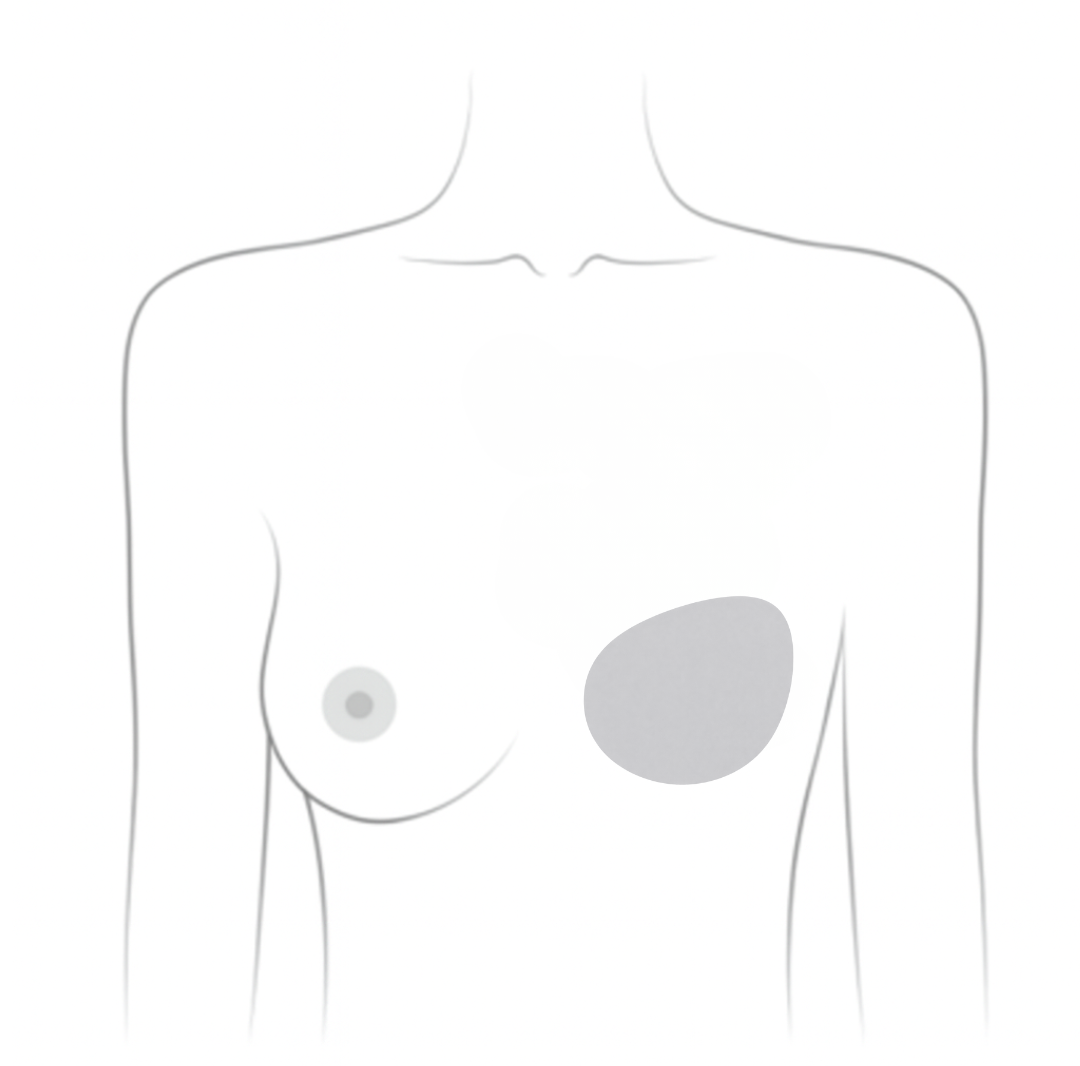
- Single mastectomy: Removes one breast
- Double (bilateral) mastectomy: Removes both breasts
- Often recommended for larger and/or more aggressive tumours
- Longer surgery and recovery time than lumpectomy, which may involve an overnight hospital stay
- May not require radiation therapy, though some still require it

“The tumour in my breast was multi focal, which means that I had more than one tumour in my breast, and the largest tumour was 3cm. Therefore, my breast surgeon highly recommended a mastectomy. I opted for a bilateral mastectomy because I was young, and symmetry on both sides was important to me.
~Trisha~
Prophylactic Mastectomy
A preventative surgery that removes both breasts to lower the risk of developing breast cancer
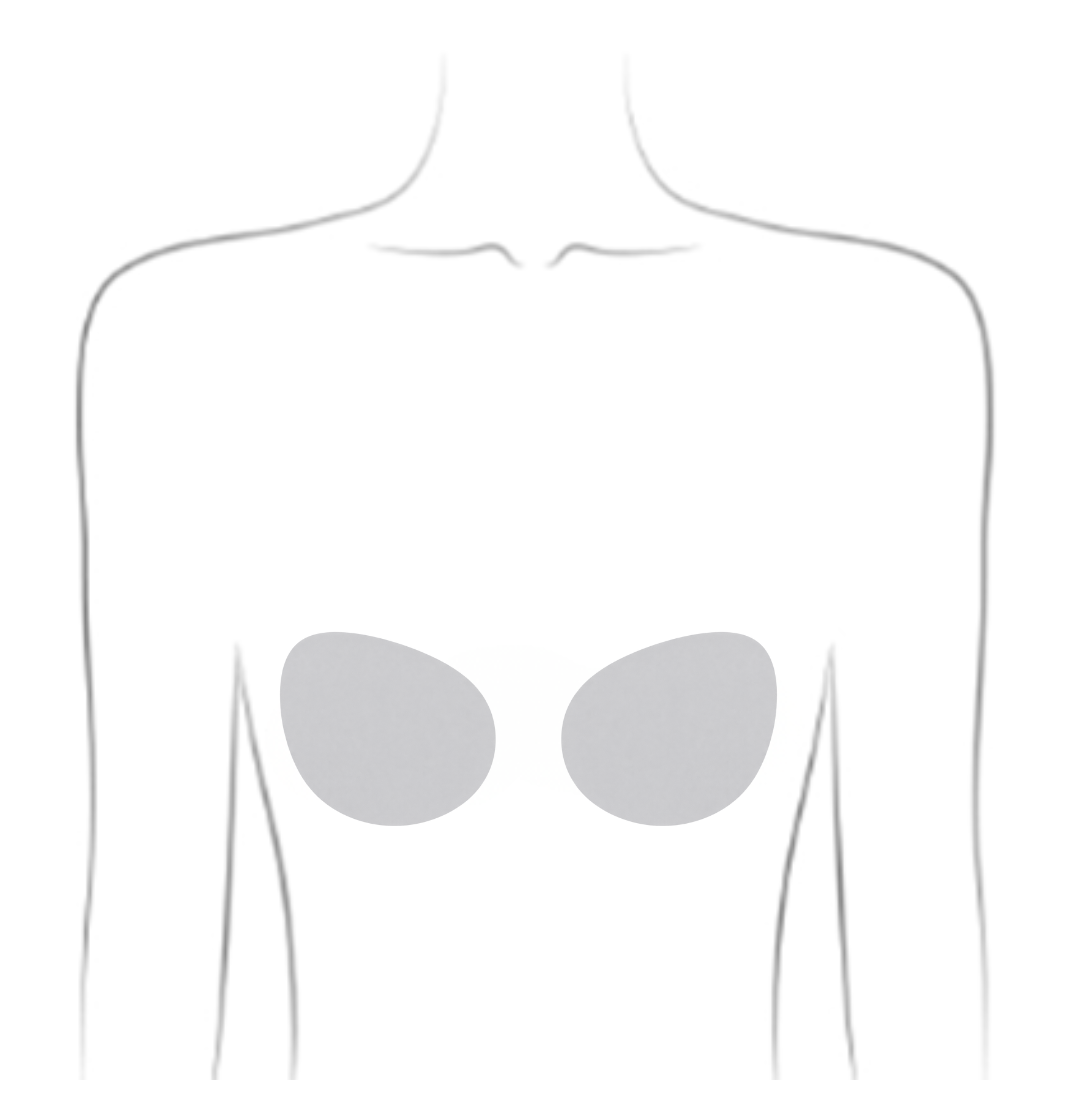
- Considered for BRCA1 or BRCA2 mutation carriers to reduce breast cancer risk
- Recommended for people at high risk due to other gene mutations or extensive family history
- Patients undergoing a single mastectomy who want to reduce the risk of cancer in the other breast (Learn more about contralateral breast cancer risk)

“At the age of 18, I was diagnosed with the BRCA1 genetic mutation just as my mother, auntie, and sister before me. This meant that I was at high risk for contracting breast cancer.
~Quinn~
Medical Reviews by Siba Haykal, MD, PhD, FRCSC, FACS, October 2025 and Mark Basik, MD, FRCSC, December 2025
- References
-
Canadian Breast Cancer Network. (2022). Breast cancer and you: A guide for people living with breast cancer [PDF]. https://cbcn.ca/web/default/files/public/Reports/Breast%20Cancer%20and%20You_ENG_edit_web.pdf
Canadian Breast Cancer Network. (2020). CBCN advocacy guide: Deciding which breast cancer surgery is right for you? [PDF]. https://cbcn.ca/web/default/files/public/Reports/Advocacy%20Guide%20-%20Surgery.pdf
Canadian Cancer Society. (2024). Choosing the breast surgery that is right for you. https://cancer.ca/en/cancer-information/cancer-types/breast/treatment/surgery/choosing-the-breast-surgery-that-is-right-for-you
Conner, K., & Uscher, J. (2025). Lumpectomy. Breastcancer.org. https://www.breastcancer.org/treatment/surgery/lumpectomy
Fisher, B., Anderson, S., Bryant, J., Margolese, R. G., Deutsch, M., Fisher, E. R., Jeong, J. H., & Wolmark, N. (2002). Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. The New England Journal of Medicine, 347(16), 1233–1241. https://doi.org/10.1056/NEJMoa022152
Giannakeas, V., Lim, D. W., & Narod, S. A. (2021). The risk of contralateral breast cancer: A SEER-based analysis. British Journal of Cancer, 125(4), 601–610. https://doi.org/10.1038/s41416-021-01417-7
National Cancer Institute. (2022). Surgery choices for women with DCIS or breast cancer. National Institutes of Health. https://www.cancer.gov/types/breast/surgery-choices