By continuing to use our site, you consent to the processing of cookies, user data (location information, type and version of the OS, the type and version of the browser, the type of device and the resolution of its screen, the source of where the user came from, from which site or for what advertisement, language OS and Browser, which pages are opened and to which buttons the user presses, ip-address) for the purpose of site functioning, retargeting and statistical surveys and reviews. If you do not want your data to be processed, please leave the site.
The Voice of People With Breast Cancer
Guiding you through your breast cancer diagnosis
PatientPath
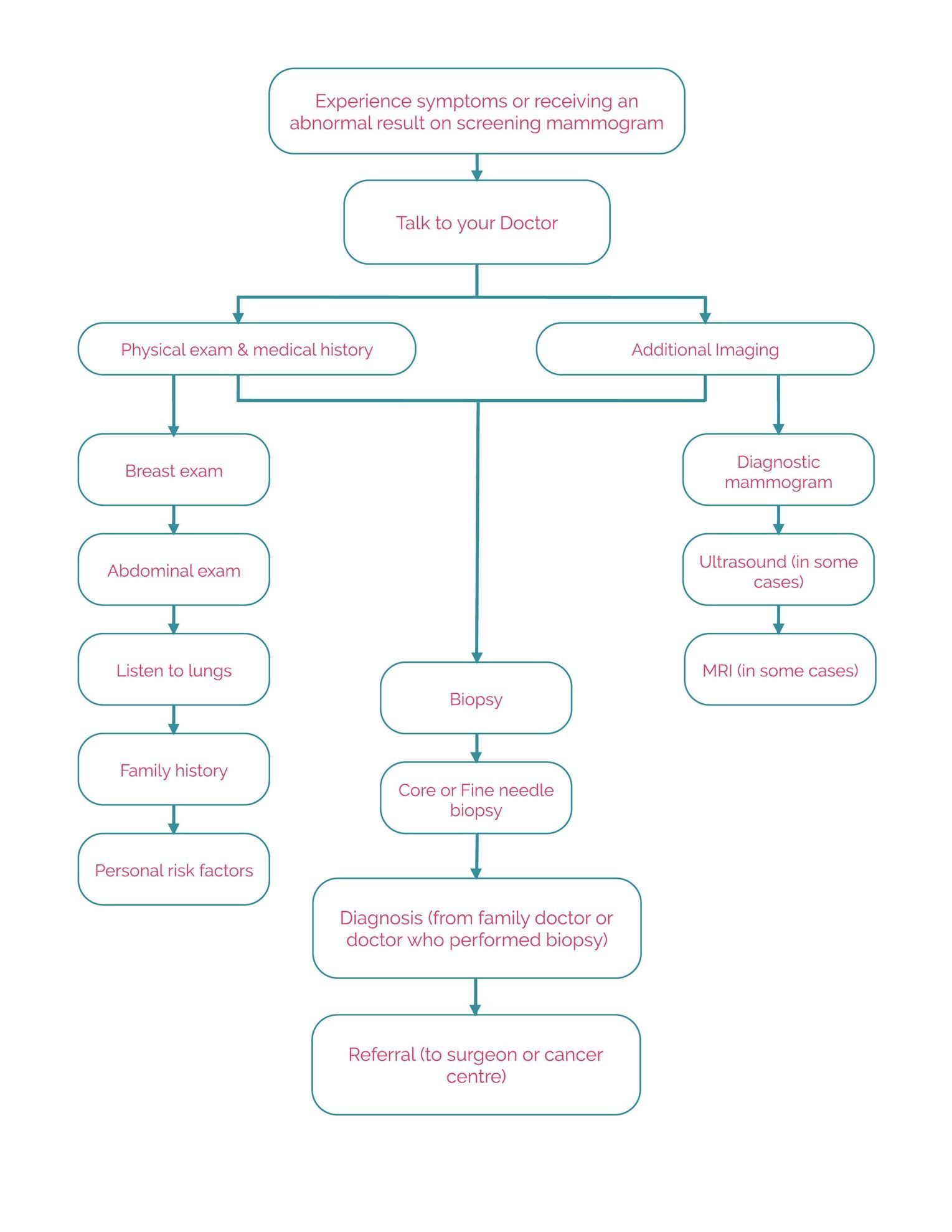
Steps to Diagnosis
Do I have breast cancer? If you have found this tool, it is likely because you or your doctor may suspect that you have breast cancer. You could be experiencing one of the following:
- You have noticed symptoms of breast cancer:
- A lump in your breast or armpit
- Unusual changes to your breast, like the size or the shape
- Changes to your nipple
- Unusual discharge from your nipple
- You’ve had a regular screening mammogram and further testing is needed
Not all breast cancers present with a noticeable lump. Invasive lobular breast cancer and inflammatory breast cancer can present with other unusual changes to your breasts. If you notice anything unusual it’s important to speak with your doctor. (For more information and resources on rare breast cancer types, visit Community Resources in Managing the Impact of Breast Cancer section.)
It is also important to remember that not all breast changes or abnormal results mean you have breast cancer. It can often mean that the doctors want to have a closer look to be sure. Getting an abnormal mammogram result or noticing changes to your breasts does not mean you automatically have breast cancer. This time of uncertainty can be scary. We are here to walk you through the next steps.
*Remember: Not all experiences may follow this exact path and you may or may not have all the tests or treatments we outline below. We hope this pathway will give you a general understanding of the process and possible timelines. We encourage you to always consult your doctor for the most accurate information and timeline specific to your circumstances.
1. Talking with your doctor
If you have noticed changes to your breast or if your mammogram results require further tests, the first thing you will do is speak with your doctor. During this appointment, your doctor may give you a full physical exam and review your medical history.
A physical exam consists of a clinical breast exam (CBE). Your doctor will carefully examine the skin on your breast and armpits and will systematically check both breasts and armpits to feel for any irregularities or lumps. They will do this while you are sitting up and then again while you are lying down.
The doctor will also likely examine your abdomen and listen to your lungs. If you are experiencing symptoms elsewhere in your body, they will examine those areas as well.
It is important to also review your medical history and discuss any potential risk factors including a family history of breast or other cancers.
Tip: Bring a list of:
- Any symptoms you are experiencing
- Medications you are taking (along with dosage amounts)
- Any family history or medical conditions you think your doctor may not be aware of
2. Imaging Tests
If your doctor determines that additional testing is necessary, he or she will make the appropriate referrals. You may be referred for any of the following additional tests:
Diagnostic mammogram: A diagnostic mammogram is used when breast cancer symptoms are present and if a change is seen on a screening mammogram. These mammograms are x-rays that create detailed images of a targeted area of the breast at different angles. It is different from a regular screening mammogram because they are attempting to get a closer look at a specific area of your breast. These appointments often take longer than regular screening because they are getting images from multiple angles. They also may be used during a biopsy.
Timeline:
- A diagnostic mammogram can take anywhere from 10 to 15 minutes to complete.
Breast ultrasound: An ultrasound uses sound waves to create images of your body – in this case, the breast. It can be used to accompany mammography imaging to give additional information about the tumour and may also be used during breast biopsies. It can also be used for women with dense breasts. Ultrasound can be useful as it can often show differences between solid masses (like tumours) and masses filled with fluid (like cysts).
Timeline:
- A breast ultrasound can take anywhere from 15 to 30 minutes to complete.
Breast MRI: An MRI (magnetic resonance imaging) is a specialized imaging machine that uses magnetic and radio waves to create detailed images of specific areas of the body – in this case, the chest. Breast MRIs are only offered in certain circumstances. It can be used for people experiencing nipple discharge, those who are considered high risk of developing breast cancer and those who are showing symptoms of distant metastases (meaning cancer is present in other areas of the body).
Timeline:
- A breast MRI can take anywhere from 30 to 60 minutes to complete.
CT scan: A CT or CAT (computerized axial tomography) scan is a 3D imaging machine that takes multiple x-rays at different angles to look at organs or abnormalities within the body. CT scans are typically only indicated if you are suspected to have stage III or IV breast cancer and are used to help rule out distant metastases.
Bone scan: A bone scan is an imaging test that looks at bone abnormalities and can help diagnose bone metastases (cancer that has spread to the bone). Bone scans are also only indicated if you are suspected to have stage III or IV breast cancer and are used to help rule out distant metastases. They can also be routinely ordered during treatment of stage IV metastatic breast cancer.
*A note on lobular breast cancer: Invasive lobular carcinoma is a type of breast cancer that does not typically form a lump. This means that it may be harder to diagnose using mammography. If you or your doctor suspect that you have lobular breast cancer, an ultrasound or MRI may be recommended.
Referral wait times: Wait times for referrals to each diagnostic test can vary widely depending on the level of urgency, type of test and province. You may get an appointment within a week, or you could be waiting several months. Ask your doctor what your level of urgency is and how long you should anticipate waiting for your referral appointment.
Tip: Follow up with your doctor’s office and the imaging centre a week later to make sure the referral was sent and received. Ask the imagining centre if there is a cancellation list you can be added to for an earlier appointment or continue to call weekly to see if there has been a recent cancellation. Some hospitals run their MRI machines 24 hours a day. If you are willing, see if there is an earlier appointment during the night.
3. Biopsies
If your imaging results come back abnormal, your doctor may send you for a breast biopsy. This biopsy will take samples of the tissue in your breast to be examined further by a pathologist. A biopsy is used as the definitive diagnosis for breast cancer.
Most biopsies are done in the hospital as a day procedure. Once the tissue has been examined, a pathology report is created. A pathology report will detail the type of cells, characteristics of the cell and if they are normal, cancerous, or abnormal but non-cancerous. To better understand your pathology report, visit www.mypathologyreport.ca.
There are different methods of biopsy commonly used to diagnose breast cancer.
Fine needle biopsy: A fine needle biopsy uses a very fine needle with a syringe to remove a sample of cells, tissue, or fluid from the breast lump. This is a minimally invasive method that may require local anesthesia and should leave no scarring. This biopsy can help determine if the mass is a cyst or a tumour but may not be able to provide any additional details about the characteristics of the cancer.
Core needle biopsy: A core needle biopsy uses a hollow needle with a syringe to remove a cylinder-shaped sample of tissue from the breast. Often, the doctor will use an ultrasound or a mammogram to help guide the needle. Like the fine needle method, this procedure may also require local anesthesia and should not leave scarring.
Side effects: Both methods may cause pain and tenderness at the injection site, along with some bleeding or bruising.
Timeline:
- Fine needle and core needle biopsies can take 15 to 30 minutes to complete.
Excisional (surgical) biopsy: This type of biopsy attempts to remove the entire lump from the breast, as well as a surrounding area of normal tissue called the margin. Since this method is more invasive, local anesthesia, sedation or general anesthesia is required, which may result in a longer recovery and may leave a scar.
Side effects: This procedure can cause pain and tenderness, along with some bleeding and bruising. The procedure may also alter the size and shape of your breast.
Wait times: Wait times for needle biopsies typically can take 3 or 4 weeks but can sometimes be weeks longer.[1],[2]
Standard of Care: A minimally invasive core needle biopsy should be performed when possible.[3]
4. Results and Diagnosis
Once the results of your tests come back and a diagnosis has been made, you will be notified by either your family doctor or the doctor who performed your biopsy. Your diagnosis may include information on:
- Staging*
- Type
- Sub-type of your cancer
- Grade
*Staging may only be determined and confirmed after you complete your breast cancer surgery. If you have been given a stage, your staging may be reassessed again after your breast cancer surgery.
Standards of Care:
- Initial results of biopsy should be reported within 7 days and include classification of sub-type.[4]
- Initial abnormal imaging results to diagnosis should take no longer than 6 weeks.[5]
If you are diagnosed with or suspected to have stage III breast cancer, you may be recommended to go for further testing to ensure the cancer has not spread to other areas of your body. These tests can include:
- Chest x-ray
- Liver ultrasound
- CT scan or MRI
- Bone scan
5. Referral to Cancer Program
After your diagnosis, your doctor will refer you to the cancer program in your community or, if you live in a remote area, to the closest hospital or centre in charge of cancer care.
If you are eligible for primary breast surgery, you will be referred to a breast cancer surgeon first. You may see a general surgeon who specializes in breast cancer surgery, or you may be seen by a surgical oncologist. Both surgeons should be highly qualified to perform your breast cancer surgery.
If you are eligible for neoadjuvant therapy (therapy completed before your surgery) or if you are not eligible for surgery, you will be referred to a medical oncologist at a cancer centre or a general practitioner in oncology. People who may be referred to a medical oncologist can include:
- People who are stage 2 or greater and have a HER2 positive or triple negative subtype
- People who are diagnosed with locally advanced stage IIIB, inoperable or inflammatory breast cancer with any subtype
- People who are diagnosed with stage IV metastatic breast cancer
For more information on stages, types and subtypes visit the Understanding My Breast Cancer section.
Standards of Care:
- Initial consultation with a breast cancer specialist should take no longer than 2 weeks from the date of your referral[6] but might be longer in some cases.
- Surgeons should have experience or up-to-date training in performing breast cancer surgeries and lymph node biopsies.[7]
[1] Ministry of Health British Columbia, Surgery wait times for Adult – Breast Biopsy https://swt.hlth.gov.bc.ca/swt/WaitTimesResults.xhtml;jsessionid=86fdca717d36be28ce2f30bd5c65?procName=Breast+Biopsy&adult=Y
[2] Ministry of Health Nova Scotia, Healthcare Wait times for Breast Biopsy (core needle) https://waittimes.novascotia.ca/procedure/breast-biopsy-needle-core#trends
[3] Canadian Partnership Against Cancer, Pan-Canadian standards for breast cancer surgery 2019, page 16 https://s22457.pcdn.co/wp-content/uploads/2019/05/Breast-Cancer-Surgery-Standards-EN-April-2019.pdf
[4] Canadian Partnership Against Cancer, Pan-Canadian standards for breast cancer surgery 2019, page 19 https://s22457.pcdn.co/wp-content/uploads/2019/05/Breast-Cancer-Surgery-Standards-EN-April-2019.pdf
[5] Canadian Partnership Against Cancer, Pan-Canadian standards for breast cancer surgery 2019, page 16 https://s22457.pcdn.co/wp-content/uploads/2019/05/Breast-Cancer-Surgery-Standards-EN-April-2019.pdf
[6] Canadian Partnership Against Cancer, Pan-Canadian standards for breast cancer surgery 2019, page 19 https://s22457.pcdn.co/wp-content/uploads/2019/05/Breast-Cancer-Surgery-Standards-EN-April-2019.pdf
[7] Canadian Partnership Against Cancer, Pan-Canadian standards for breast cancer surgery 2019, page 17 https://s22457.pcdn.co/wp-content/uploads/2019/05/Breast-Cancer-Surgery-Standards-EN-April-2019.pdf
- You have noticed symptoms of breast cancer: