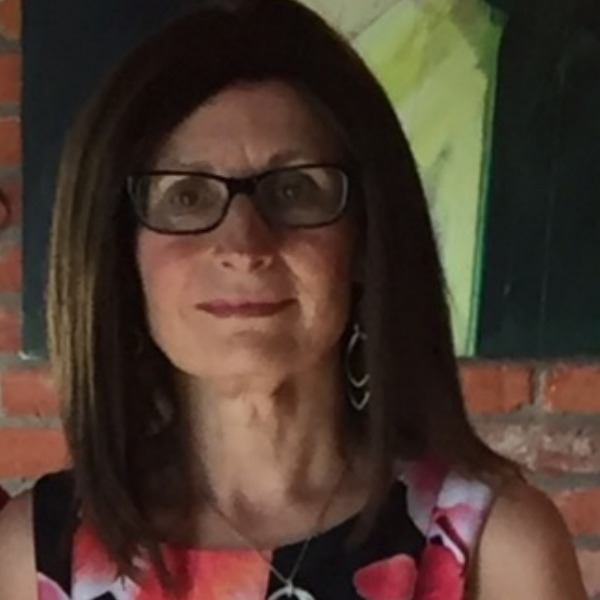
By Carmela Bocale
 I was not prepared for the number of decisions regarding treatment that needed to be made from cancer diagnosis to treatment options. It was both exhausting and overwhelming – how does one make sound life-changing decisions when there are so many options and choices? I learned to trust myself and be my own advocate as I navigated through the many decision points.
I was not prepared for the number of decisions regarding treatment that needed to be made from cancer diagnosis to treatment options. It was both exhausting and overwhelming – how does one make sound life-changing decisions when there are so many options and choices? I learned to trust myself and be my own advocate as I navigated through the many decision points.
Fundamental to that was having an amazing support network, as I did (it’s foundational), but at the end of the day you have to make the decision that is best for you and you have to do it for you – not for anyone else. My support network included the most loving partner, my mom, my sisters, my boys, my daughter-in-law, and my granddaughter, so many friends, and a remarkable employer who supported my time away from work financially through our sick leave plan and supported medications and treatments that were not covered in the provincial medical plan.
I realize I’m very fortunate and that not all women have these resources and supports in place. We need to do what we can, whether that is through education, advocacy, support networks, and financial and emotional support to ensure all women have treatment options that support their overall well-being.
Though I won’t be able to tell my full story in this blog, what I do want to share is how I become my own advocate to manage the many symptoms that came along with the treatment options and how I decided to manage those side-effects:
Resiliency: When navigating through a cancer diagnosis, there are so many things that are out of your control. I so desperately wanted to focus on what I could control, and what was essential was my choice to be resilient. Resiliency doesn’t mean being a “Pollyanna” or not acknowledging your emotions. It is about having a number of strategies in place to navigate through this life-changing experience.
Education and Research: I researched various cancer-related sites and supports dedicated to education. I did a lot of reading and attending educational webinars (Inspire Health, CBCN, just to name a couple—there are lots of good ones) to determine the best way to manage symptoms and the many decisions I had to make.
Physiotherapy: I educated myself about the physical side effects of my mastectomy, which included tenderness, limited arm or shoulder movement, and numbness in my chest and upper arm – particularly where the lymph nodes were removed. What I discovered through my research is the necessary exercises to reduce these symptoms. Prior to surgery, I investigated physiotherapy options and had that in place so that I could transition to physiotherapy following the recovery from surgery. I was dedicated to my exercises and to my therapy sessions. I also explored what exercises to do to reduce lymphedema and am mindful of limitations. Today I still have some numbness, which will probably never go away, but I have full-range arm movement, which is a result of being committed to my physiotherapy and exercises following my surgery.
Acupuncture: The hot flashes were fast and furious once I started chemotherapy. Because of the type of breast cancer I had, estrogen and progesterone receptor positive, there was nothing I could take to help, but what did help was acupuncture!! Initially I went twice a week for four weeks and now I’m on monthly maintenance. This was a life saver!
Diet and Exercise: Managing the many side effects of chemotherapy was difficult at times but I was able to cope through nutrition and exercise (yes, the medications also help). I stayed away from alcohol for the whole time, enjoyed protein shakes in the morning and did my best to stay focused on unprocessed foods. Plenty of water was essential.
Physical exercise: To manage the exhaustion during chemo, I incorporated a daily walk. Even when I couldn’t get off the couch (and it was hard most days), my support was there to make sure I went for a walk. What a difference that made! Walking also helped me sleep better, and when you sleep better, it just makes a positive difference.
Following chemotherapy was the decision to take tamoxifen. The side effects hit me hard. They included bone pain and aches, and overall energy depletion (also due to the after-effects of chemotherapy). I was back at work when I started tamoxifen, so a combination of all that I had to manage that year, a very demanding work role, and then medication that affected me so physically was a lot to take. So much so that I really didn’t have the energy to even consider doing anything about it. I was like this for about two years, and then I finally had had enough. I was tired of saying I’m tired and I was frustrated that I was unable to get up off the floor when playing with my granddaughter. I was feeling so exhausted that I couldn’t exercise, which wasn’t helping with my overall mental health.
Finally, I did research on food and inflammation and I had a light bulb moment. I thought, “That is what my problem is: inflammation. It’s why I can’t move!” I decided to do an elimination diet and removed gluten, dairy, sugar, eggs, and corn to see if it would make a difference. Within days I could move again – I could not believe it. I was slowly getting my energy back and then moving more (doing more exercise) which gave me even more energy! And I lost some weight along the way (bonus). I gradually introduced some things back into my diet over a few months and determined that I could not tolerate gluten (joint pain reduced) or dairy (less stomach problems). Sugar also bothers me and depletes my energy but that has been harder to give up (as I write this I’m eating dark chocolate.) I’m a work in progress.
Supplements: Another outcome of the treatments is brittle nails. My nails have never been the same and I don’t know if they ever will be. I recently started to take collagen supplements in my daily protein shake in hopes that they will help. I also regularly take calcium, magnesium. a probiotic, and vitamin D and am exploring adding fish oil.
Put it on Hold: I had a reconstruction surgery date booked and then I cancelled – I have decided I’m not ready for further surgery and maybe I never will be and that is okay.
Taking control of what I could to gain normalcy in my life made a difference to me and my overall well-being and has helped me to be resilient and remain hopeful each day. I haven’t stopped exploring more options to help me manage ongoing symptoms: next is yoga and meditation. I’m a work in progress and committed to taking control of what I can!