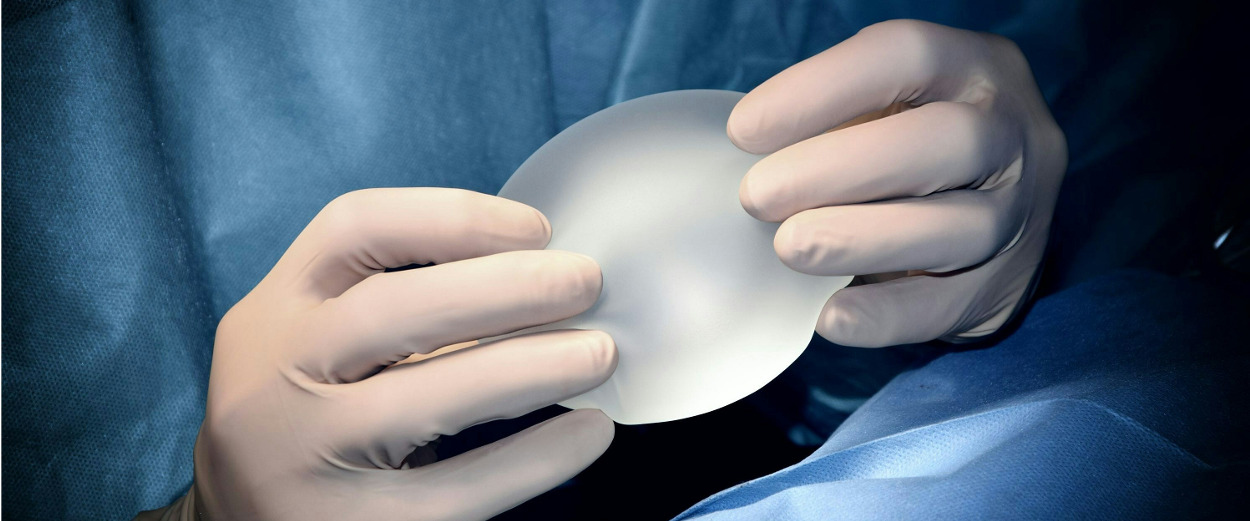
In the 1960s silicone gel breast implants came into use, allowing for breast reconstruction post-mastectomy or augmentation to be possible, but at that time, there was no clear standard for the implant placement. At first, surgeons placed the prosthesis in front of the chest (pectoralis major) muscle, but the chance of postoperative complications was high. These issues included necrosis of the skin flap (where the skin tissue dies due to a lack of blood supply), infection, and other problems such as external exposure of the implant, capsular contracture (where the breast hardens around the implant) and rippling on the skin surface.
These complications arose because there was not enough tissue covering the area properly, and so reconstruction techniques changed from prepectoral implant placement to subpectoral. The subpectoral method places the implant completely or partially under the chest muscle while still keeping the muscle attached to the chest wall. While being reliable and safer, this method also had its drawbacks; contraction of the muscle could result in pain due to muscle spasms as well as animation deformity. This is a phenomenon where the chest muscle contracts, pushing the implant upwards and distorting the shape of the breast mound. Subpectoral placement of the implant could also prevent lower pole expansion (how the breast naturally hangs), resulting in poor shape and definition. Placing the implant partially under the chest muscle from the bottom results in a more natural hanging shape. However, this technique may also lead to a phenomenon called “window shading”, where the edge of the chest muscle becomes visible across the implant when strongly contracted.
With advancements in plastic surgery and breast reconstruction techniques and materials, prepectoral implants have resurged in popularity. One of the major contributors to the success of modern prepectoral reconstruction was the use of acellular dermal matrix (ADM). First used on burn victims in the 1990s, ADM is a biosynthetic material derived from humans, pigs, or cows. It works like a scaffold for new tissues to grow on and adhere to during the healing process. ADM was first used in breast reconstruction in the early 2000s. A pocket of ADM is created, into which the implant is sewn or wrapped. It is then inserted under the mastectomy skin flap, on top of the chest muscle, and sutured in place. This lowered the risks associated with subpectoral implantation, as well dramatically improved the results that surgeons had in the 1960s and 70s with prepectoral implants, as the pocket of ADM works as a protective extra layer of soft tissue under the mastectomy skin flap.
Your surgeon can advise whether prepectoral implant placement is an option for you based on certain factors, including the amount and condition of the breast tissue that remains after mastectomy. Sometimes, one to three fat-grafting treatments at some point after implant reconstruction surgery may be recommended to help thicken the soft tissue layer over the implant and prevent wrinkling and rippling.