By continuing to use our site, you consent to the processing of cookies, user data (location information, type and version of the OS, the type and version of the browser, the type of device and the resolution of its screen, the source of where the user came from, from which site or for what advertisement, language OS and Browser, which pages are opened and to which buttons the user presses, ip-address) for the purpose of site functioning, retargeting and statistical surveys and reviews. If you do not want your data to be processed, please leave the site.
The Voice of People With Breast Cancer
helping you understand your surgical options
SurgeryGuide
Jump to:
Autologous Reconstruction
Autologous reconstruction, also called flap reconstruction, uses tissue from another part of your body (like your belly, back, buttocks, or thighs) to rebuild your breast. Unlike implant reconstruction, flap surgery creates a breast shape using your own fat, skin, and sometimes muscle. It can be done at the same time as a mastectomy (immediate reconstruction) or later (delayed reconstruction).
Why Choose Flap Reconstruction?
Many people feel that flap reconstruction offers a more natural look and feel than implants. Because it uses your own tissue, the breast may change along with your body over time. For some, this option can also avoid risks tied to implants, such as rupture or capsular contracture. However, flap surgery is usually a longer and more complex operation, with recovery involving both the chest and donor site where the flap is obtained.
Types of Autologous Reconstruction
There are several flap options, depending on where the tissue comes from and whether muscle is involved. Each type has its own benefits, drawbacks, and recovery considerations.
-
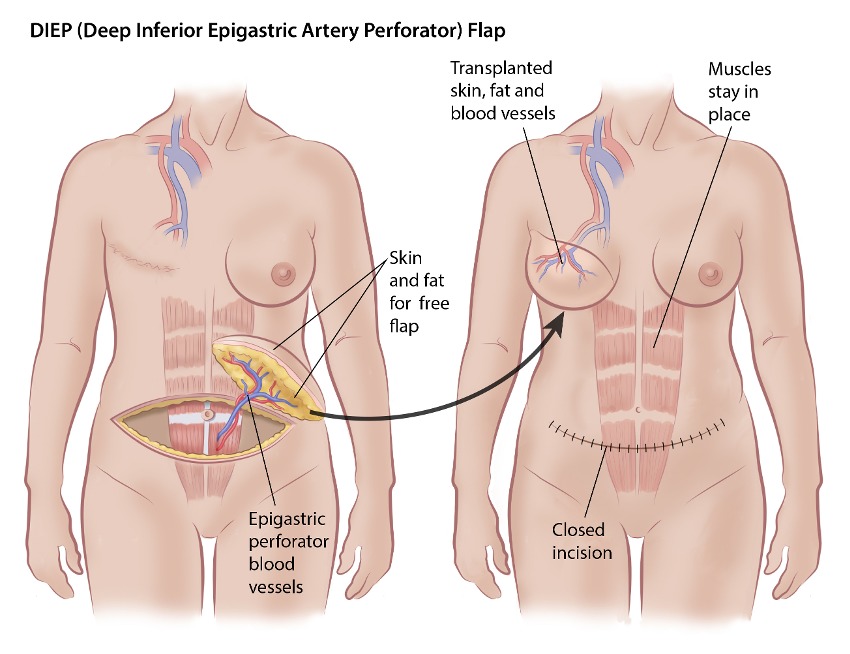
DIEP Flap (Deep Inferior Perforator Flap)
The DIEP flap is one of the most common and modern types of flap surgery. It uses excess fat and skin from the lower abdomen (similar to a tummy tuck) but does not use muscle.
The tissue is completely detached and reattached to new blood vessels in the chest using microsurgery, so this procedure requires a surgeon with specialized training and experience.
Considerations
- No muscle removal but the vessels are followed within the muscle
- Natural look and feel
- Lower risk of abdominal weakness than older methods (like TRAM flap)
- Longer, more complex surgery requiring microsurgery
- Leaves a horizontal scar along the bikini line
- Not usually an option if you do not have enough abdominal fat
- Not possible if you have had a tummy tuck and may not be possible with previous or major abdominal surgeries
View before-and-after photos of real people: DIEP Breast Reconstruction Photo Gallery. (content warning)
 “I had DIEP reconstruction, that did not involve moving any of my abdominal muscles but did include a tummy tuck and the manufacture of a new tummy button. I also had to have a follow up surgery to reduce the size of my "normal" breast and give it a "perk me up", which I believe is all done in one surgery now. For me it meant another trip to Winnipeg. After all was healed, I had another trip to make a nipple and then another one to tattoo color around it. My challenges were mostly the trips in and out and the mental issues, ie: once you start on the journey you need to complete it and sometimes you wonder why you started.
“I had DIEP reconstruction, that did not involve moving any of my abdominal muscles but did include a tummy tuck and the manufacture of a new tummy button. I also had to have a follow up surgery to reduce the size of my "normal" breast and give it a "perk me up", which I believe is all done in one surgery now. For me it meant another trip to Winnipeg. After all was healed, I had another trip to make a nipple and then another one to tattoo color around it. My challenges were mostly the trips in and out and the mental issues, ie: once you start on the journey you need to complete it and sometimes you wonder why you started.I am generally pleased with the result. It is not identical to my normal breast but then I am the one who knows this. In my bra/swim suit or clothes no one else could tell. I do like being rid of the prostheses.
I had no complications at all and was treated with respect by all the health care providers.”
~Sheila~ -
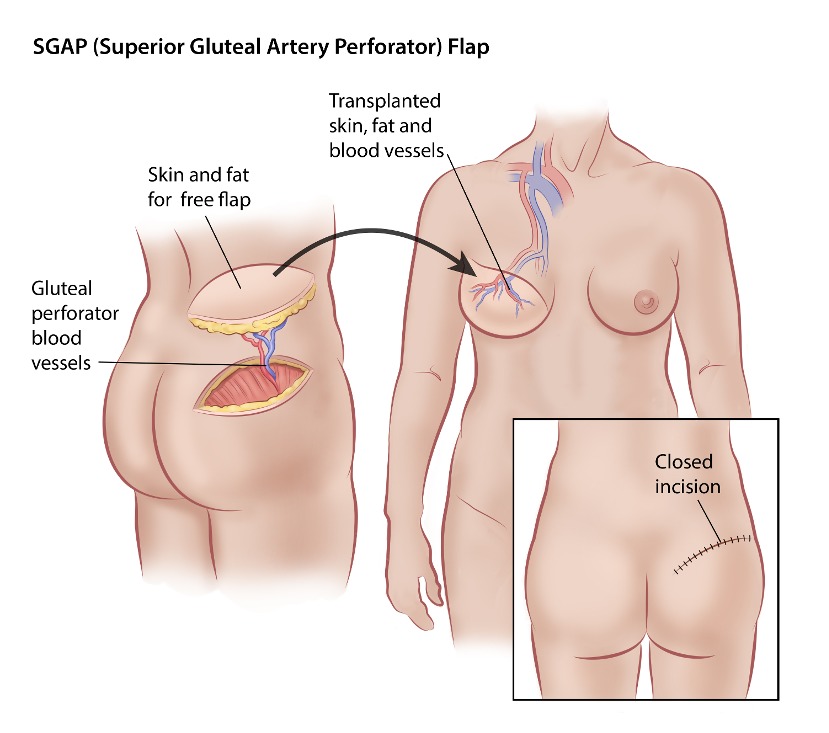
SGAP (Superior Gluteal Artery Perforator)
The SGAP flap uses skin and fat from the upper buttock area to reconstruct the breast and does not use any muscle.
Considerations:
- No muscle removal
- Ideal when abdominal tissue is unavailable or unsuitable
- No impact on core strength compared to other options
- Does not take fat from lower buttocks, reducing discomfort when sitting
- A complex procedure, requiring microsurgery
View before-and-after photos of real people: SGAP Breast Reconstruction Photo Gallery. (content warning)
-
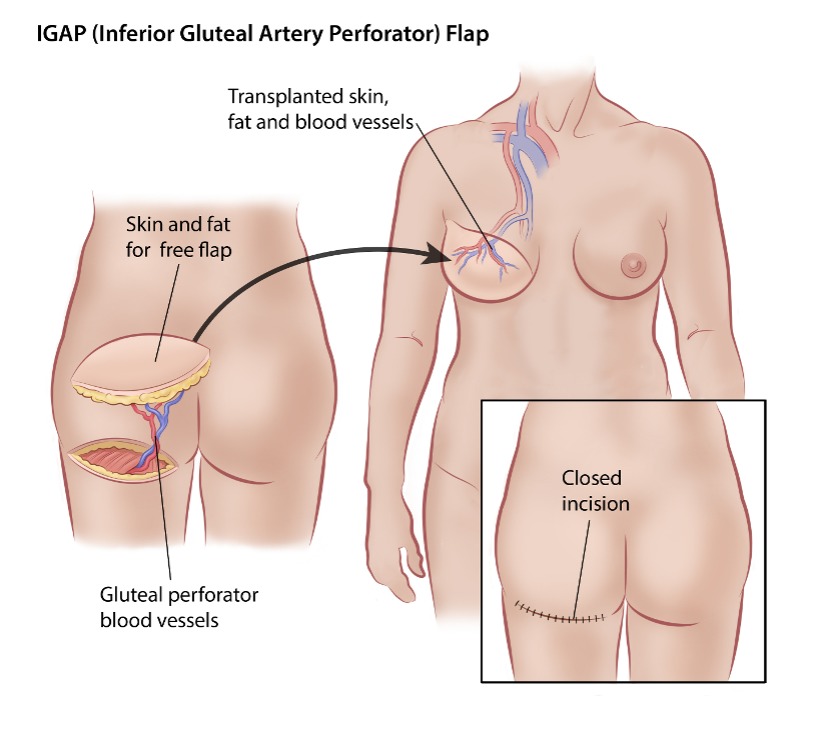
IGAP (Inferior Gluteal Artery Perforator)
The IGAP flap uses skin and fat from the lower buttocks to reconstruct the breast, without removing muscle.
Considerations:
- No muscle removal
- Scar placed in the buttock crease, usually hidden
- May slightly reduce the size or shape of the buttocks
- Higher risk of donor site complications compared to other flap types
- Can make sitting uncomfortable during recovery
- Less common than SGAP
View before-and-after photos of real people: IGAP Flap Before and After Photo Gallery (content warning)
 “I was young and felt reconstruction was right for me. I would change my choice now, I had an IGAP flap and I think the recovery would have been easier with an implant. Recovery would have been easier, knowing what I know now. Having one surgical site to recover from would have been faster and easier on my body. With the surgery site being an IGAP flap, it meant not being able to sit for almost 4 weeks. It made day-to-day tasks complicated, things, like sitting on the toilet or sitting at the dinner table, were impossible.
“I was young and felt reconstruction was right for me. I would change my choice now, I had an IGAP flap and I think the recovery would have been easier with an implant. Recovery would have been easier, knowing what I know now. Having one surgical site to recover from would have been faster and easier on my body. With the surgery site being an IGAP flap, it meant not being able to sit for almost 4 weeks. It made day-to-day tasks complicated, things, like sitting on the toilet or sitting at the dinner table, were impossible. There were a few appointments after surgery that were required, as I was to have chemotherapy. Getting in a car was a challenge. As well, getting up and onto the scanning machines was also hard. Most technicians had not seen the surgery I had and it was imperative my husband help me onto the tables. I would not trust anyone else at that time.
As well, I had a 10 and 12-year-old at home. I laid in bed for 4 weeks and had limited mobility. They were used to seeing me up and at the gym. I could not do much around the house and that made it more apparent that I was sick. It certainly took a toll on my family. I feel going straight to an implant would have been a speedier recovery, with less scarring on my body.”
~Tara~ -
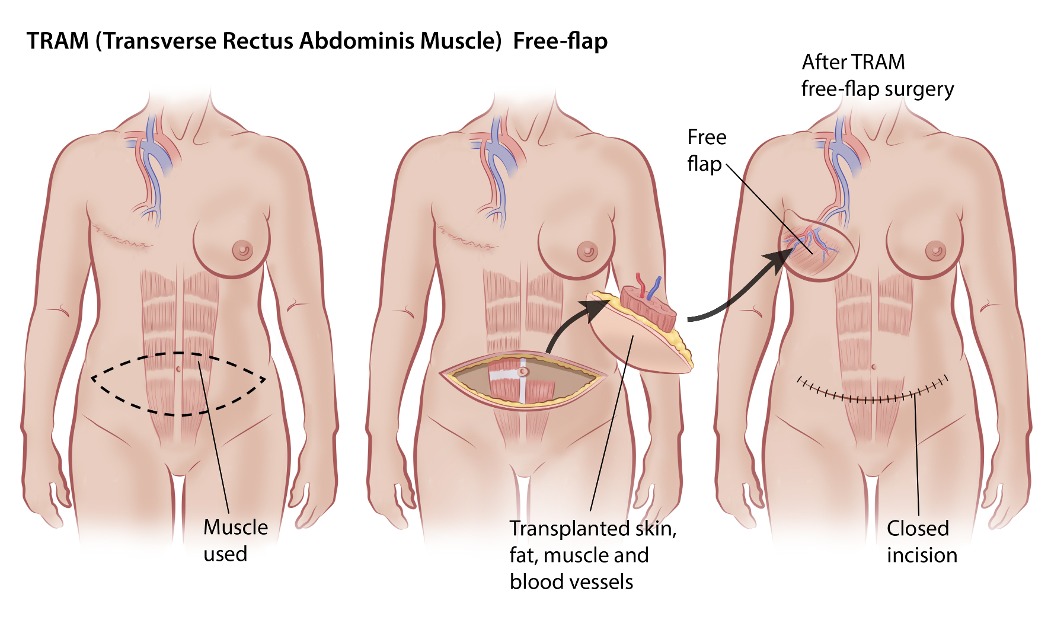
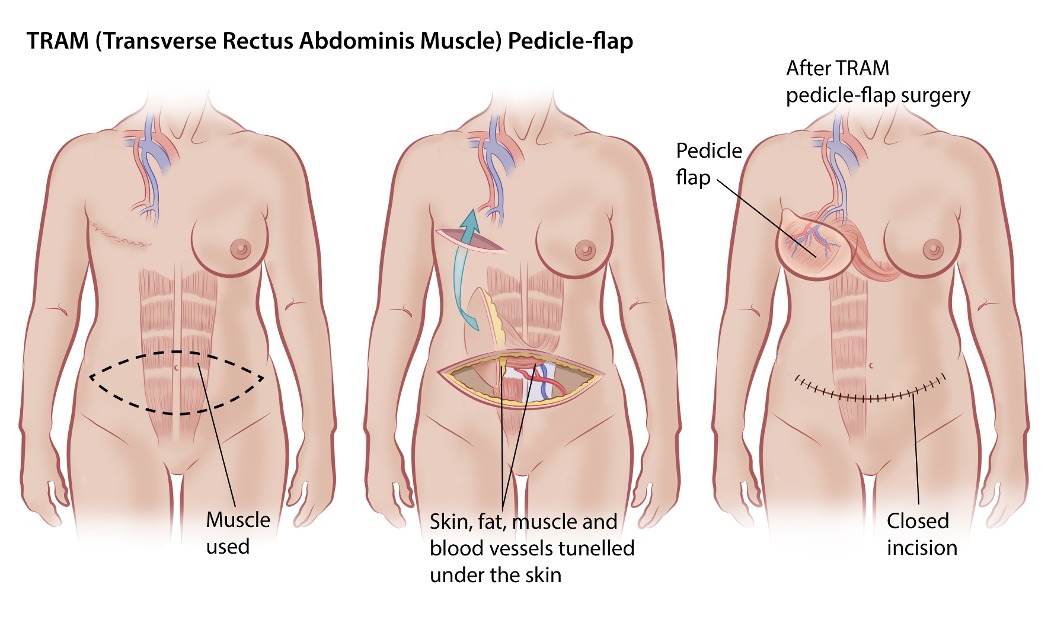
TRAM flap (transverse rectus abdominis)
The TRAM flap uses skin, fat, and part of the rectus abdominis muscle from the lower abdomen to reconstruct the breast.
Considerations:
- Because muscle is removed, recovery can take longer and core strength may be affected
- Free TRAM uses less muscle than pedicle TRAM, potentially reducing complications
- Not a good choice if you do not have extra belly tissue or if you have already had many abdominal surgeries
- Shorter surgery time than DIEP but requires microsurgery
- If the whole muscle is removed, a mesh will be used to strengthen your abdomen and help prevent abdominal weakness
View before-and-after photos of real people: TRAM Flap Before and After Photo Gallery. (Content warning)
 “I had a TRAM reconstruction after right sided mastectomy. I developed seromas in my abdominal site that had to be drained every month for six months. After three months they tried putting in a new drain but it got infected almost right away and I was on antibiotics for two weeks. Then three months later they admitted me to hospital and opened up the abdominal donor site and apparently the abdomen was "a mess" as the mesh that the doctor used to strengthen my abdominal wall had not integrated into the surrounding tissue and actually broke down into fragments that all had to be removed during a long surgery.
“I had a TRAM reconstruction after right sided mastectomy. I developed seromas in my abdominal site that had to be drained every month for six months. After three months they tried putting in a new drain but it got infected almost right away and I was on antibiotics for two weeks. Then three months later they admitted me to hospital and opened up the abdominal donor site and apparently the abdomen was "a mess" as the mesh that the doctor used to strengthen my abdominal wall had not integrated into the surrounding tissue and actually broke down into fragments that all had to be removed during a long surgery. Once that issue was cleared up and my abdomen healed all was well. My left breast, which was lifted and reduced, healed very well and looks fantastic. The reconstructed breast also healed well and both breasts match and look like the "real" thing. I did have a nipple constructed using the origami technique. This lost its profile after a year. I then got the plastic surgeon to inject it with restylane. This lasted a couple of years but then it also flattened out and I was at the point after a few years where I didn't really want to have anymore interventions and ceased to care about having "one headlight" as my husband says. I found a nipple cover at a lingerie store which does the trick when I have on thin tops.
I would say that beside the side effects of the mesh in my abdomen, the other most disconcerting issue was loss of sensation in my entire trunk. It's very difficult emotionally waking up to the reality of having your entire torso, which used to be sensitive to the touch, to be completely numb. I only had sensation in one breast and then my right breast and entire torso down to my pubic area felt dead to me. That sounds harsh but it took me quite awhile to not be saddened by that loss of sensation. It definitely has an impact on your sex life. When you run your own hand over your tummy and not really have a sense of where your hand is if you're not looking...that was hard. It has taken years to regain sensation in that area despite being told it might only be five years. It's now 12 years since my surgery and I can feel most of my torso except for a 4" circumference around my umbilicus. And of course no sensation in my reconstructed breast, which some women have said they regained. Not me.
I was very happy to wake up from surgery with two breasts that matched, were reduced and lifted after losing some of that youthfulness, and I had a tight and flat tummy. Despite not being over-weight, I still had a post baby tummy so it was very cool to wear tight jeans and tight tees again after all these years. If I could promise a woman that she wouldn't have the issues with seromas that I had, I would highly recommend immediate reconstruction after a mastectomy. I actually felt quite sexy despite losing the sensation in that one breast, just in terms of my outside appearance. I also loved having my own tissue in my new breast...it really feels just like a "real" breast with breast tissue. It moves like the other one and if I lose weight so does my chest, and if I gain weight so do my breasts. They look very natural.
I think it's really important, especially if you love the touch of your hand or your lovers touch to know that there is an entire erogenous zone from your neck to your pubic area that is numb for many years to come. I think there are more advanced surgeries for woman who need a mastectomy and want reconstruction that don't result in the cutting of so many nerves in your abdomen. I would seek out those practitioners who are doing that kind of surgery. I loved using my own tissue as opposed to having a foreign body inside me, but I think the loss of sensation to your torso is a big price to pay for many years.”
~Colleen~ -
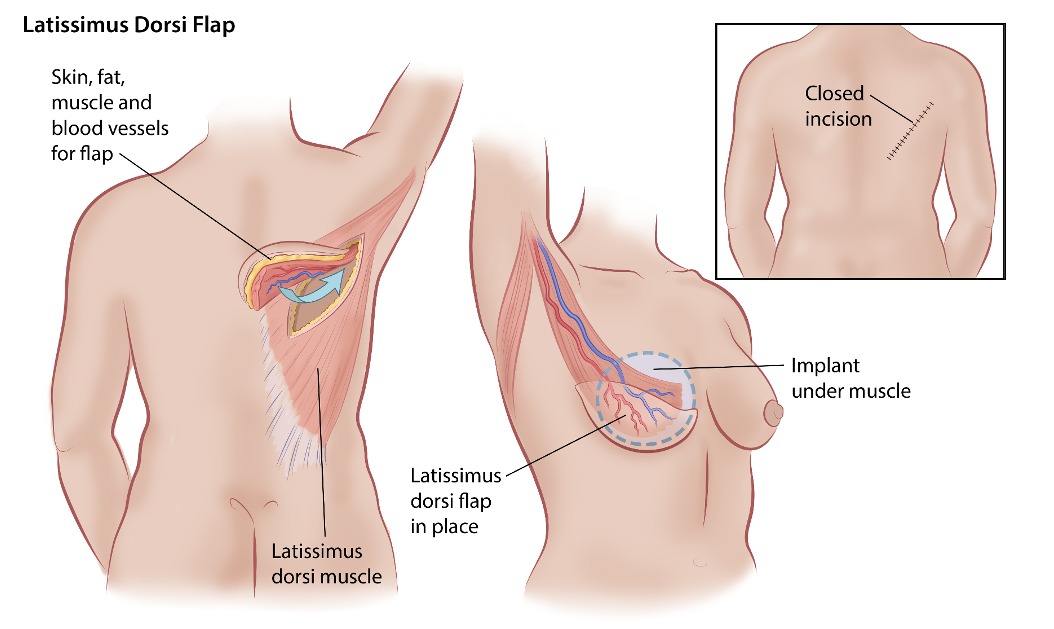
Latissimus Dorsi Flap
This technique uses skin, fat, and the latissimus dorsi muscle from your upper back to rebuild the breast. This flap is typically used in combination with a tissue expander implant.
Considerations:
- Suitable for small to medium reconstructions
- Used when other flaps are not an option
- Significant amount of muscle is used
- Muscle loss may affect shoulder function
View before-and-after photos of real people: Latissimus Flap Before & After Photo Gallery. (Content warning)
 “After speaking with my plastic surgeon about the various options that were available to me, I made an informed decision to get the latissimus dorsi flap reconstruction done. I had already gone through radiation which caused changes in the elasticity of my skin and also had a history of infection from my lumpectomy one year prior. By doing the latissimus dorsi flap, it would help minimize the risk of infection and allow for more skin elasticity and a more desired outcome by using healthy tissue from my back.
“After speaking with my plastic surgeon about the various options that were available to me, I made an informed decision to get the latissimus dorsi flap reconstruction done. I had already gone through radiation which caused changes in the elasticity of my skin and also had a history of infection from my lumpectomy one year prior. By doing the latissimus dorsi flap, it would help minimize the risk of infection and allow for more skin elasticity and a more desired outcome by using healthy tissue from my back. I was grateful to have a surgeon who explained the process in great detail but also spent a lot of time on the internet doing my own research so I knew what to expect. I also spoke to other women who had been through it and could provide valuable insight as to their own first-hand experience with this type of reconstruction. I think it's important to have as many resources as possible and helps make things a little less scary when you know what to expect. One thing I did not expect though was the significant loss of feeling in my back where the skin and tissue was removed. Although some of the feeling has returned, there will always be a loss of sensation which is troubling sometimes.
Was I pleased overall with the results? Yes and no. While my right affected (cancer) breast looked and felt more natural than expected, my non-affected side was the problem child. I had gaps and indents along my breast and a loose pocket of skin underneath that didn't get filled out from the expansions. I have come to learn though that breast reconstruction is never a perfect process and it can take time (and a lot of patience) to get the results to where you want them to be.
I think it's really important for others to be prepared going into a surgery like this. The healing time is significant and it is hard to go about your daily activities for at least a couple of weeks. Having a good support system lined up is key to helping do things like making dinner, walking the dog, taking kids to school and cleaning around the house. I had meals prepped beforehand and items on hand that would help keep me comfortable during recovery like a drain dolly to hold the multiple drains in one place, a pillow to stick under each arm for bed or while resting on the couch, and a seatbelt pillow for the car.”
~Kim~ “One thing that might be good for others to know is the back may feel very numb for a very long time ... I always describe it like feeling like a piece of wood - it can take a couple of years for all the feeling to return to the area. If there is any feeling in the area it should all return eventually. This surgery sounds very daunting but I found it pretty easy to recover from and have no restriction in movement due to this surgery.
“One thing that might be good for others to know is the back may feel very numb for a very long time ... I always describe it like feeling like a piece of wood - it can take a couple of years for all the feeling to return to the area. If there is any feeling in the area it should all return eventually. This surgery sounds very daunting but I found it pretty easy to recover from and have no restriction in movement due to this surgery.Another thing to be aware of is a small possibility of capsular contracture happening with any permanent implant - this just happened to me and I had surgery to exchange the implant in January. Breast reconstruction can be as easy as one surgery but it can mean several surgeries over time; however everyone I know is happy they had it done, including me. I have met many, many women who either wish they had had reconstruction or wish they had been offered reconstruction, it just makes you feel normal again.
Every woman should at the very least be given all of her treatment options at the time of her diagnosis. I had the best possible care and given every option and my mission is to help all women who have not been as fortunate as I have been. I have been extremely pleased with the results.
~Susan~ “Its been just over a year since I had the implants put in and honestly I don't like the feeling of them. They feel like a foreign object that now is a part of me. On the side where they removed the cancer, it causes me the most problems while moving certain ways. I was going to go back to the surgeon and let him know, however a bone scan that was done last month showed Costochandral inflammation in the chest and rib on the right side, this is due to previous rib fractures.
“Its been just over a year since I had the implants put in and honestly I don't like the feeling of them. They feel like a foreign object that now is a part of me. On the side where they removed the cancer, it causes me the most problems while moving certain ways. I was going to go back to the surgeon and let him know, however a bone scan that was done last month showed Costochandral inflammation in the chest and rib on the right side, this is due to previous rib fractures. After my double mastectomy the plastic surgeon put in my expanders in the same surgery. Every 3 weeks I went to the plastic surgeon and he would give me my CC's of fluid to fill the expanders. The surgery was June 23 and by Nov, I had my last one and then I ended up in emergency in horrible pain a few days later. Apparently the last amount of fluid was too much for me and it was resting on my diaphragm. A few days later the surgeon drained me on the one side and it gave me instant relief.
We then went to plan B which was the flap surgery where they took about 9 inches in the width of my back and brought that skin and tissue to the front. My back has never been the same since. They look good but there is so much numbness in both the front and the back of me. I was warned it would be like this. The flap surgery affects a lot of the nerves and I’m left with what feels like to me a block of wood in my back. Like something that doesn't belong there. My range of motion has been affected too. I think that is the scar tissue.
I’m pleased with the look of the implants and I now have a perfect size C. I don’t have to wear a bra, so some good things did come out of this.
I would want others to know that you have to expect to have weird feelings with the implants as they do feel odd, like something is just sitting there on your chest. And that it wasn't until I had the nipple tattoos, that I finally felt I looked whole again and 1/2 normal. I’m still very shy around my husband. I still hide from him. I feel abnormal. I guess it’s the scars, the implants and the fake nipples make me feel not real anymore. Yet on the other hand, in the mirror I look okay.”
~Cheryl~ “I had the Dorsi Flap procedure done, muscle was taken from the back and moved to the front. Expanders were put in and for six months, every second week I would have saline injections to stretch the skin. The biggest challenge was the recovery time after the initial surgery. It was a hard surgery that I wasn’t properly made aware of. Surgery was harder than anticipated and recovery time was longer than expected. I would recommend the full year wait after the mastectomy to ensure you are ready, mentally and physically.
“I had the Dorsi Flap procedure done, muscle was taken from the back and moved to the front. Expanders were put in and for six months, every second week I would have saline injections to stretch the skin. The biggest challenge was the recovery time after the initial surgery. It was a hard surgery that I wasn’t properly made aware of. Surgery was harder than anticipated and recovery time was longer than expected. I would recommend the full year wait after the mastectomy to ensure you are ready, mentally and physically. I was encouraged to go earlier as the hospital had some cancellations before the Christmas season; which was a bad idea. I was not well enough to enjoy Christmas that year and recovery time was way underestimated by the surgeon. I found the first few fills very painful but got much more tolerable as time went on and also had smaller fills.
I was pleased with the results, the surgeon did a great job. I waited a couple of years and am now ready for the final procedures, tattoo and nipple reconstruction. Was physically tired of surgeries after the expanders were removed and the inserts put in. It was a hard surgery and I’m glad now that it is over. Sometimes I felt the surgery was harder than the cancer treatments.
My advice would be to do your research and get best option for your body type. Have a couple pieces of clothing with inside pockets (many sports tops/hoodies have them); they were a life savers to carry around the drains in the incisions”
~Corinne~ -
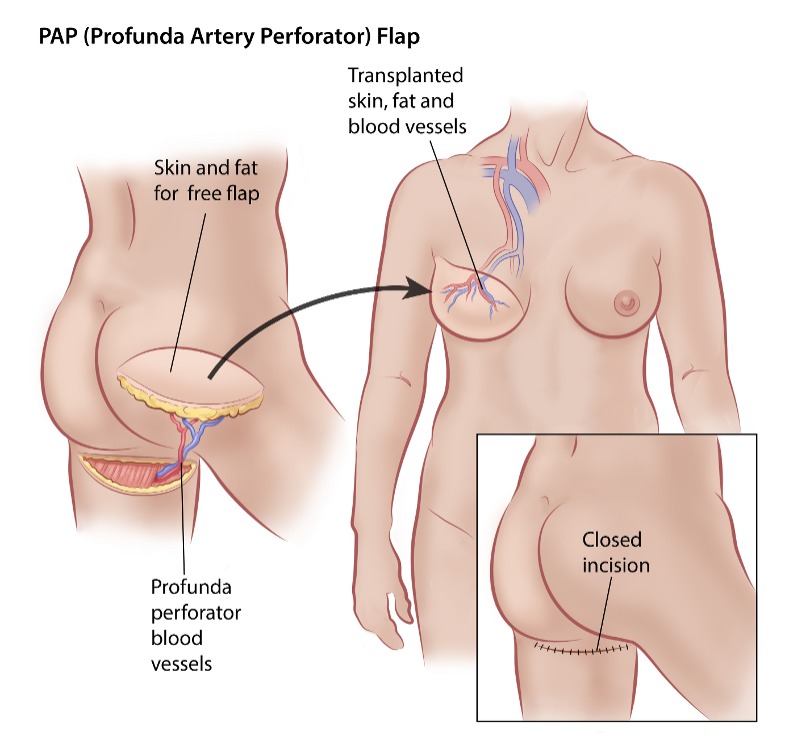
PAP Free Flap (Profunda Artery Perforator Flap)
The PAP flap uses skin and fat from the upper inner or back of the thigh to reconstruct the breast, without removing any muscle.
Considerations:
- No muscle removal
- Ideal for small to medium-sized reconstructions
- A good option for those with limited abdominal tissue
- Scar is usually hidden in the inner thigh crease
- Microsurgery needed and less widely available
View before-and-after photos of real people: PAP Flap Reconstruction Before and After Photo Gallery. (Content warning)
-
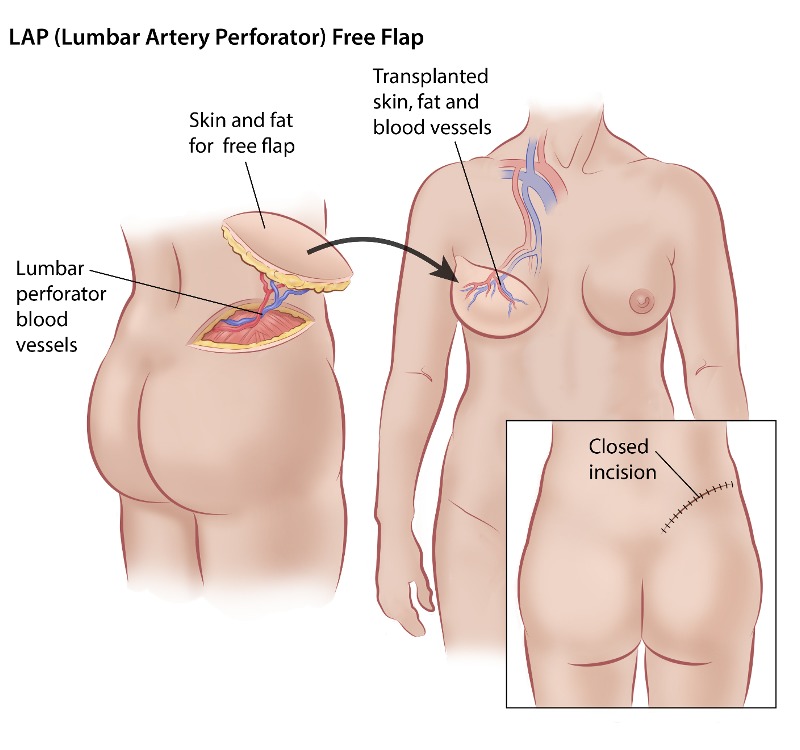
LAP Free Flap (Lumbar Artery Perforator Flap)
The LAP flap uses skin and fat from the lower back and upper buttocks (the "love handles") to reconstruct the breast, without removing any muscle. This flap provides natural shaping due to the quality and density of the fat in the donor area.
Considerations:
- No muscle removal
- Provides a natural shape due to the quality and density of the fat used
- Ideal for those who aren't candidates for abdominal flaps (like DIEP)
- Fat from this area allows for easier breast shaping
- Less commonly offered, complex surgery requiring microsurgery
View before-and-after photos of real people: LAP Flap Before & After Photo Gallery. (Content warning)
-
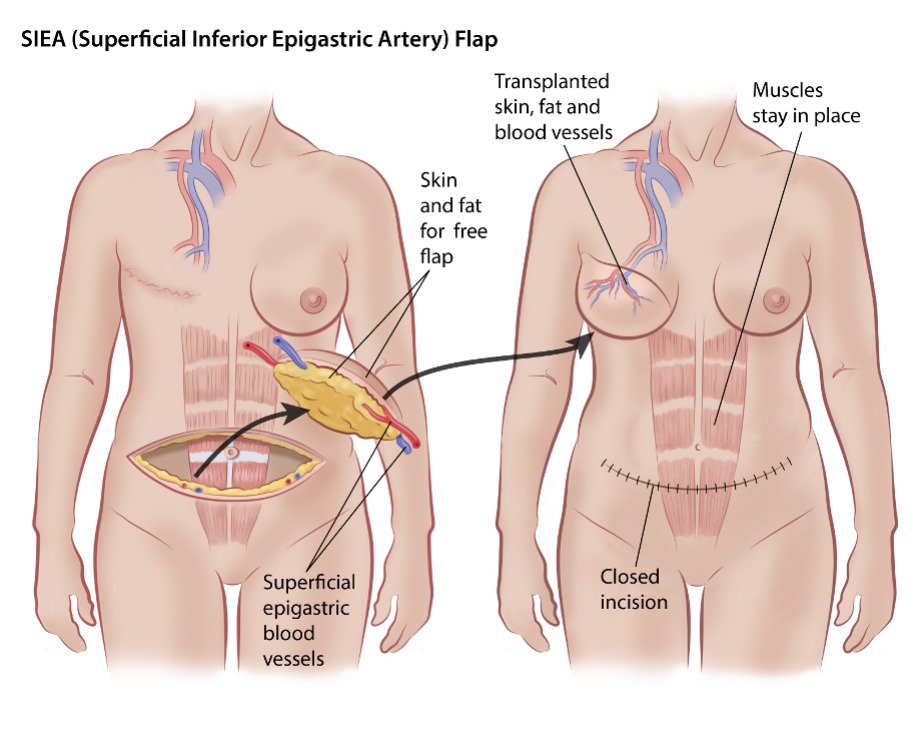
SIEA Flap (Superficial Inferior Epigastric Artery)
The SIEA flap reconstructs the breast using fat from the lower abdomen without cutting into abdominal muscle or its covering tissue. It uses a different set of blood vessels than the DIEP flap, and the strength of your blood supply often determines which is recommended.
Considerations:
- No muscle removal
- No loss of core strength
- Not always possible depending on your anatomy
- Less invasive than DIEP but less commonly performed
View before-and-after photos of real people: SIEA Flap Reconstruction Before and After Photo Gallery. (Content warning)
Sensation Loss and New Techniques
Loss of feeling in the reconstructed breast is common after flap surgery. The donor site may also be numb or feel strange. While some sensation may return over time, it often does not come back fully.
Newer techniques like flap neurotization, where nerves are reconnected during reconstruction, are showing promise in restoring some feeling to the chest. If preserving or regaining sensation is important to you, ask your surgical team whether this option is available.
- References
-
American Cancer Society. (2021). Breast reconstruction using your own tissues (flap procedures). https://www.cancer.org/cancer/types/breast-cancer/reconstruction-surgery/breast-reconstruction-options/breast-reconstruction-using-your-own-tissues-flap-procedures.html
Breastcancer.org. (2023). Capsular contracture. https://www.breastcancer.org/treatment/surgery/breast-reconstruction/corrective-reconstruction/capsular-contracture
Breast Cancer Now. (2023). Breast reconstruction using your own tissue. https://breastcancernow.org/about-breast-cancer/treatment/surgery-for-primary-breast-cancer/breast-reconstruction/breast-reconstruction-using-your-own-tissue
Canadian Breast Cancer Network. (2022). Breast cancer and you: A guide for people living with breast cancer [PDF.] https://cbcn.ca/web/default/files/public/Reports/Breast%20Cancer%20and%20You_ENG_edit_web.pdf
Cho, M. J., Schroeder, M., Flores Garcia, J., Royfman, A., & Moreira, A. (2025). The current state of the art in autologous breast reconstruction: A review and modern/future approaches. Journal of Clinical Medicine, 14(5), 1543. https://doi.org/10.3390/jcm14051543
Conner, K. (2023). TRAM flap reconstruction procedure. Breastcancer.org. https://www.breastcancer.org/treatment/surgery/breast-reconstruction/types/autologous-flap/tram
Curtis, A. (2024). Flap reconstruction surgery (autologous reconstruction). Breastcancer.org. https://www.breastcancer.org/treatment/surgery/breast-reconstruction/types/autologous-flap
Levine, J. L. (n.d.). IGAP flap before and after photo. Center for Breast Reconstruction. https://centerforbreastreconstruction.com/portfolio-items/igap-before-after-photo-by-dr-joshua-l-levine-662007/
Levine, J. L. (n.d.). PAP flap reconstruction before and after photo. Center for Breast Reconstruction. https://centerforbreastreconstruction.com/portfolio-items/pap-flap-reconstruction-photo-mk/
Momeni, A., Meyer, S., Shefren, K., & Januszyk, M. (2021). Flap neurotization in breast reconstruction with nerve allografts: 1-year clinical outcomes. Plastic and Reconstructive Surgery. Global Open, 9(1), e3328. https://doi.org/10.1097/GOX.0000000000003328
Northwest Breast Center. (n.d.). Photo gallery: DIEP breast reconstruction. https://www.northwestbreastcenter.com/diep-breast-reconstruction
Perimeter Plastic Surgery. (n.d.). Latissimus flap pictures. https://www.perimeterplasticsurgery.com/before-and-after-pictures/breast-reconstruction-before-and-after-photos/latissimus-flap-before-after-pictures/
Perimeter Plastic Surgery. (n.d.). TRAM flap pictures. https://www.perimeterplasticsurgery.com/before-and-after-pictures/breast-reconstruction-before-and-after-photos/tram-flap-pictures/
The Center for Restorative Breast Surgery. (n.d.). SGAP breast reconstruction result photos. https://www.breastcenter.com/result-photos/sgap-photos/
The Plastic & Reconstructive Surgery Group. (n.d.). Before & after photographs. https://tprsg.com/photos/diep-flap/case-15
The Plastic & Reconstructive Surgery Group. (n.d.). Before & after photographs. https://tprsg.com/photos/sgap-flap/case-37
Yale Medicine. (2022). Microsurgery: What you need to know. https://www.yalemedicine.org/news/microsurgery-what-you-need-to-know